Session Information
Date: Sunday, October 26, 2025
Title: (0233–0279) Miscellaneous Rheumatic & Inflammatory Diseases Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Cannabis use has increased substantially in the past decades, with legalization expanding across the U.S. Despite its known therapeutic potential, the immunomodulatory effects of cannabis remain unclear. Prior studies suggest cannabis may influence immune responses, potentially affecting autoimmune disease risk. However, epidemiological evidence on its long-term impact on autoimmune disease incidence is limited. We evaluate the association between cannabis, use and the incidence of autoimmune diseases, inflammatory markers, and major adverse health outcomes, including all-cause mortality and cardiovascular events, using a large-scale retrospective cohort analysis.
Methods: A retrospective cohort study was conducted using TriNetX Global Collaborative Network data. Two cohorts were defined: cannabis users (ICD-10: F12) and non-users, matched 1:1 via propensity scoring based on demographics, comorbidities, and social determinants. The primary outcomes included the incidence of autoimmune diseases (e.g., rheumatoid arthritis), inflammatory markers (CRP, ESR), major adverse cardiovascular events (MACE), and all-cause mortality. Statistical analyses included risk ratios, Kaplan-Meier survival analysis, and t-tests for laboratory outcomes.
Results: Among 229,366 matched patients, cannabis use was associated with a lower incidence of certain autoimmune conditions, including Hashimoto’s thyroiditis (RR: 0.512, p < 0.001), rheumatoid arthritis (RR: 0.817, p = 0.020), type 1 diabetes (RR: 0.810, p = 0.002), and vitiligo (RR: 0.735, p = 0.046). (Figure 1.) However, inflammatory markers (CRP, ESR) were significantly elevated in cannabis users (p < 0.001), and cannabis use was linked to an increased risk of MACE (RR: 1.195, p < 0.001) and all-cause mortality (RR: 1.670, p < 0.001). (Figure 2.)
Conclusion: Cannabis use was associated with significantly increased inflammatory markers, higher risk of major adverse cardiovascular events (MACE), and elevated all-cause mortality. While there appeared to be a decreased incidence of certain autoimmune diseases among cannabis users, this finding should be interpreted with caution. The lower observed rates may reflect underdiagnosis or underreporting, potentially influenced by changing patterns of healthcare engagement amid rising cannabis legalization and widespread use. As cannabis use becomes increasingly normalized, it is essential to critically evaluate both its potential harms and the risk of diagnostic oversight. Prospective research is needed to clarify causality and guide evidence-based clinical and public health recommendations.
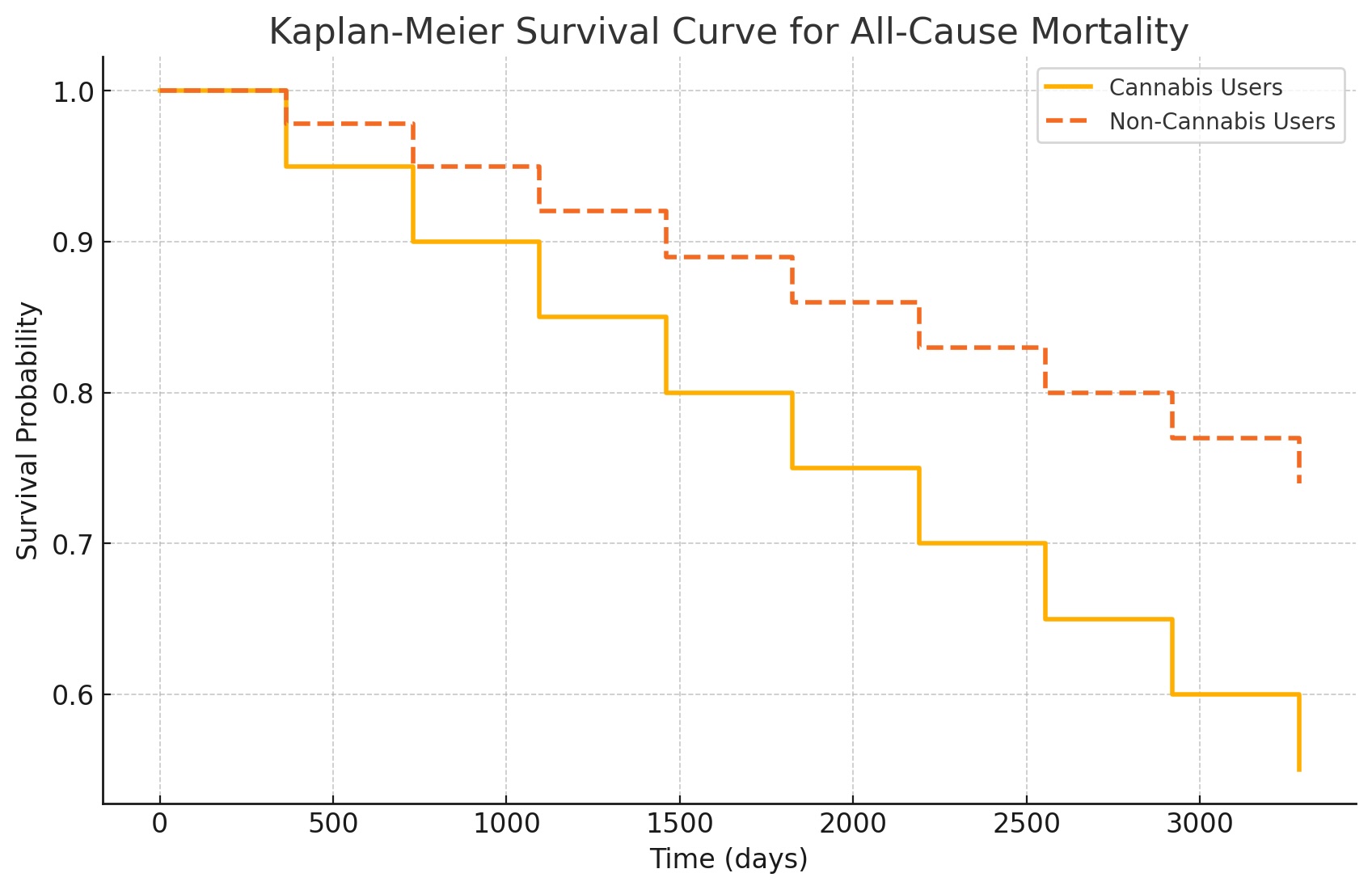 Figure 1. Forest Plot of Outcomes
Figure 1. Forest Plot of Outcomes
.jpg) Figure 2. Kaplan-Meier Curve for All Cause Mortality
Figure 2. Kaplan-Meier Curve for All Cause Mortality
To cite this abstract in AMA style:
Lam J, Otabor E, Alomari L, Kosak Lopez E, Barnett M, Abdollahi S. Clearing the Smoke: Association Between Cannabis Use and Autoimmune Disease Incidence in a Retrospective Cohort Analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/clearing-the-smoke-association-between-cannabis-use-and-autoimmune-disease-incidence-in-a-retrospective-cohort-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clearing-the-smoke-association-between-cannabis-use-and-autoimmune-disease-incidence-in-a-retrospective-cohort-analysis/
