Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Session Type: Poster Breakout Session
Session Time: 5:10PM-5:40PM
Background/Purpose: Due to the lack of widely accepted diagnostic criteria or disease biomarkers, chronic non-bacterial osteomyelitis (CNO) remains a diagnosis of exclusion. Whole-body MRI (WB-MRI) has become one of the mainstays in supporting the diagnosis of CNO. The aim of our study was to create a scoring system (MRI-score), based on recently developed scoring tool for MRI CROMRIS (Chronic nonbacterial Osteomyelitis MRI Scoring), which allows a standardized reporting of WB-MRI in order to obtain a tool useful for the staging of the disease and for the follow up.1 We evaluate correlation of our MRI-score with clinical activity parameters and with the response to treatment.
Methods: We analyzed 76 patients that met the criteria proposed by Jansson et al. for the diagnosis of CNO2. We collected at baseline (T0), before starting any treatment, clinical and radiological findings. Clinical disease activity was evaluated using a Physician’s Global Assessment (PGA). WB-MRI images were assessed using the CROMRIS as published by Zhao Y et al. According to CROMRIS, parameters included in our MRI-score were: 1) presence of bone marrow hyperintensity on STIR images, 2) signal extension, 3) presence of soft tissue/periosteal hyperintensity, 4) presence of bony expansion, 5) presence of vertebral collapse. These parameters were evaluated for each bone units grading a score from 0 to 7. In 46 of the 76 patients MRI-score, the main clinical parameters (PGA, pain VAS, ESR and CRP) and the response to therapy was evaluated also at 6 and 12 months (T6 and T12) following baseline.
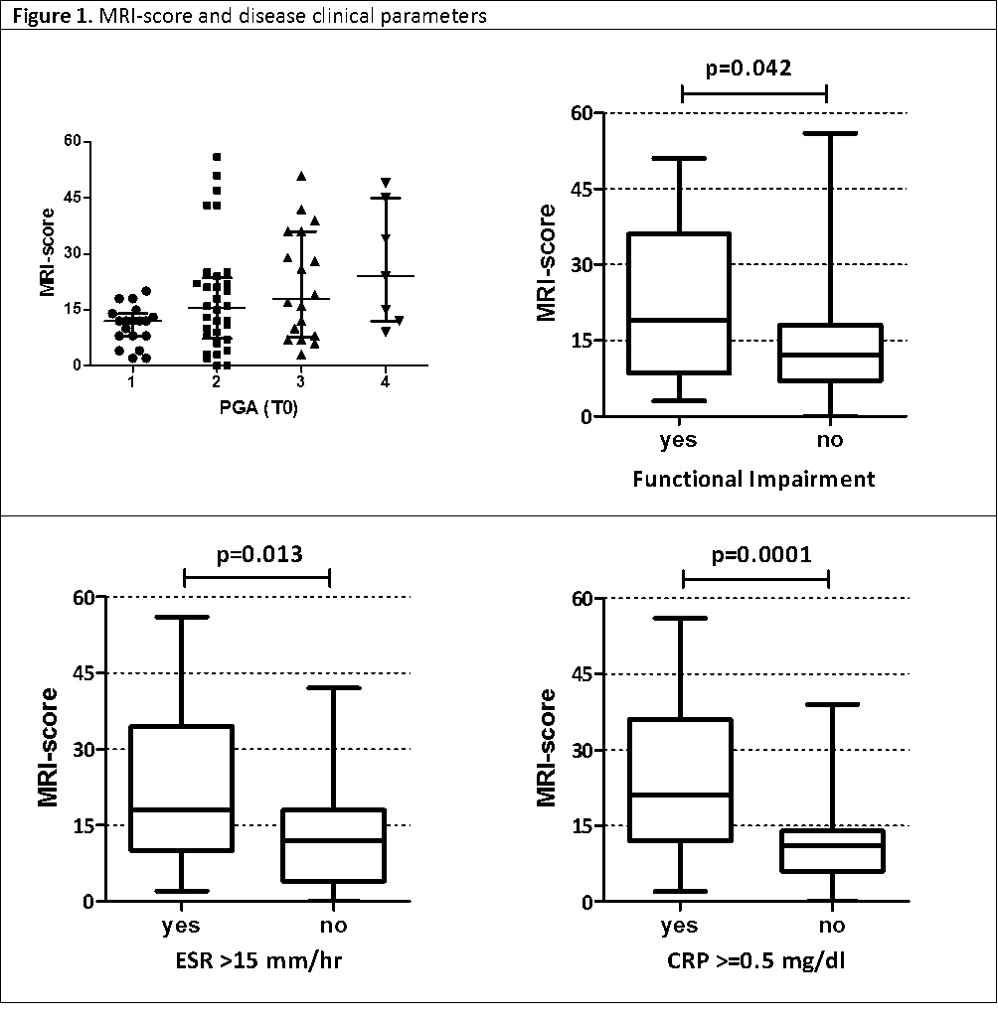
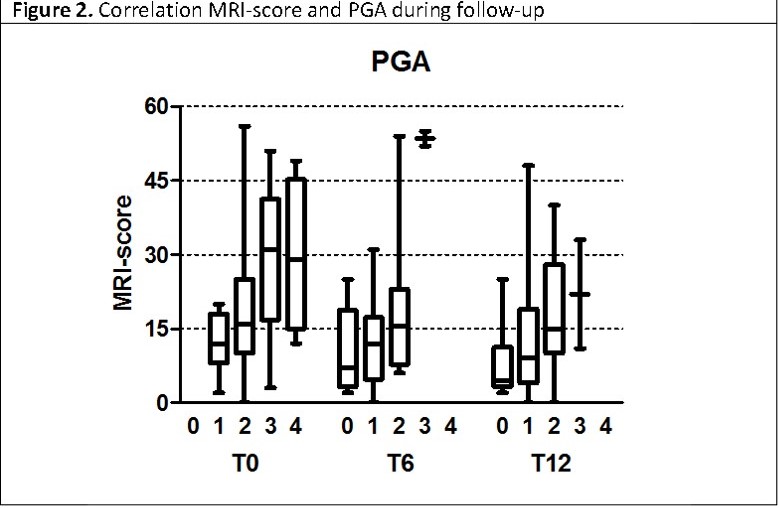
Results: A significant association between the MRI-score and some disease clinical parameters (PGA, presence of functional impairment, abnormal ESR and CRP level) was found in the 76 patients at baseline (figure 1). Among 46 patients followed for 12 months, the MRI-score, PGA, pain VAS, ESR and CRP showed a decreasing trend after 6 months from baseline that remained substantially stable at 12 months. Moreover a significant correlation between the MRI-score and the PGA was observed at baseline (p=0.0044; rho=0.41), but not at T6 and T12 (figure 2). Furthermore, patients who received bisphosphonates as first-line therapy showed a substantial decrease of the MRI-score at T6 compared to T0 (figure 3). In these patients the MRI-score was significantly higher compared to patients who received other treatment at baseline (p=0.0078).
Conclusion: In conclusion our MRI-score offers a standardized reporting system which, together with the clinical evaluation, may contribute to the diagnosis of CNO patients. Moreover, the proposed MRI-score may represent a valid tool to stratify patients with CNO based on the severity of the disease and consequently to guide the most appropriate therapeutic choice. Finally, MRI-score, allowing an objective evaluation of the effectiveness of different treatments, could possibly be included into recommendation of management of patients with CNO.
1 Zhao Y et al. J Rheumathol. 2019
2 Jansson AF et al. Arthritis Rheum. 2009
To cite this abstract in AMA style:
Capponi M, Pires Marafon D, Rivosecchi F, Pardeo M, De Benedetti F, Insalaco A. Chronic Non-bacterial Osteomyelitis (CNO): Correlation Between Clinical and Radiological Findings [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/chronic-non-bacterial-osteomyelitis-cno-correlation-between-clinical-and-radiological-findings/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/chronic-non-bacterial-osteomyelitis-cno-correlation-between-clinical-and-radiological-findings/