Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Session Type: Poster Breakout Session
Session Time: 4:30PM-5:00PM
Background/Purpose: Intrathoracic involvement in adults with systemic lupus erythematosus (SLE) is relatively common, particularly pleural disease. The prevalence of intrathoracic involvement in childhood-onset SLE (cSLE) is unclear, and screening usually is performed only when respiratory symptoms arise. Computed tomography (CT) is the most sensitive non-invasive technique for detecting intrathoracic manifestations in SLE. The purpose of this study was to investigate the frequency of intrathoracic manifestations on CT in cSLE and to examine associations between these manifestations and other disease-related variables.
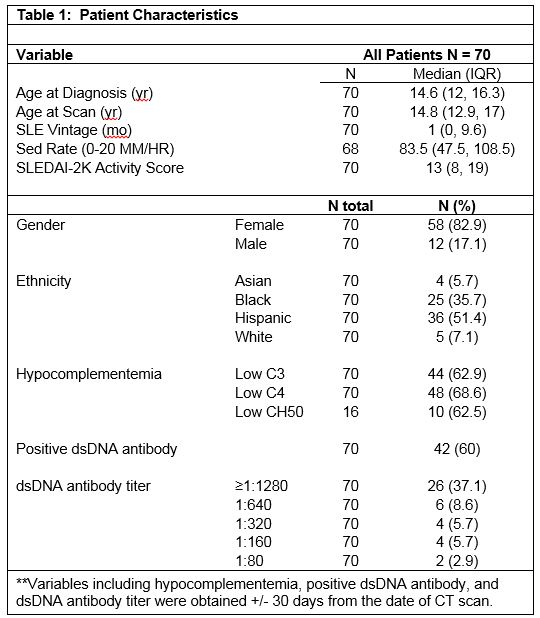
Methods: Seventy patients with initial chest CT and a new diagnosis of cSLE from 2013-2018 at Texas Children’s Hospital were included in this retrospective study. Chest CTs were included if obtained within 1 year of diagnosis or any time after diagnosis of cSLE. Chest CTs were obtained secondary to cardio-respiratory indications. 5 patients were excluded based on age >18 years old at time of diagnosis of cSLE, CT scans more than 1 year prior to date of diagnosis of cSLE, or lack of data. CT scans were assessed for serositis (pleural or pericardial effusion), pulmonary parenchymal disease (consolidation, ground glass opacities, nodules, septal thickening, cysts, fibrosis), bronchiectasis, pulmonary artery enlargement, pulmonary embolism, and hilar/mediastinal lymphadenopathy by an experienced pediatric chest radiologist without knowledge of the patients’ clinical signs/symptoms or laboratory test results. Patient characteristics were summarized using mean with standard deviation, median with 25th and 75th percentiles, and frequency with percentage. Manifestations were compared by outcomes using t-test, Wilcoxon ranksum test, Chi-square test and Fisher’s exact test. All analyses were performed using Stata v15.
Results: Patient characteristics and CT manifestations are presented in Tables 1 and 2, respectively. Out of 70 patients, 44.3% (n= 31) had serositis, 48.6% (n= 34) had pulmonary parenchymal disease, and 42% (n = 29) had hilar/mediastinal lymphadenopathy. Serositis was associated with higher SLEDAI-2K activity scores (median 18 (IQR 12-25) vs. 10 (4-16), p=0.002) when compared to all patients without serositis. While serositis was associated with dsDNA positivity (77 vs 46%) and higher titers (p=0.018), patients with pulmonary parenchymal disease had significantly lower dsDNA positivity. Patients with hilar/mediastinal lymphadenopathy had significantly higher SLEDAI-2K activity scores (median 16, IQR (10-28), p=0.02) and were more likely to have hypocomplementemia than patients without adenopathy on chest CT (median 10, IQR (5-18.5), p=0.02).
Conclusion: Consistent with prior studies of SLE, serositis was common in our pediatric SLE population. Results indicate a higher frequency of serositis and pulmonary parenchymal disease captured by CT in our cohort than previously reported in cSLE. There is a significant association between serositis and SLEDAI-2K, as well as, serositis and dsDNA autoantibodies. Additionally, findings suggest that most pulmonary manifestations in our cSLE cohort occur early in the disease course.
To cite this abstract in AMA style:
Patel P, Orman G, Silva Carmona M, Pereira M, De Guzman M, Guffey D, Wenderfer S, Guillerman R. Chest Computed Tomography Manifestations in Childhood-Onset Systemic Lupus Erythematosus: A Single-Center Cohort Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/chest-computed-tomography-manifestations-in-childhood-onset-systemic-lupus-erythematosus-a-single-center-cohort-study/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/chest-computed-tomography-manifestations-in-childhood-onset-systemic-lupus-erythematosus-a-single-center-cohort-study/