Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: It has been proposed that SLE may be divided into Type 1 and Type 2 states. Type 1 manifestations are well captured in disease activity scores (e.g. SLEDAI-2K). Type 2 manifestations include fatigue, pain, depression, brain fog. These do not always correlate with conventional lupus disease activity, but can be pervasive and dominate in patient-reported outcomes (PROs). Patients may be classified into four disease states: Minimal (low type 1 activity, low type 2 activity), High Type 1 (high type 1 and low type 2), High Type 2 (low type 1, high type 2) and Mixed (high type 1 and high type 2). Our primary aim was to define the prevalence of patients who can be classified into the four states. Our secondary aim was to identify variables that predict each disease state.
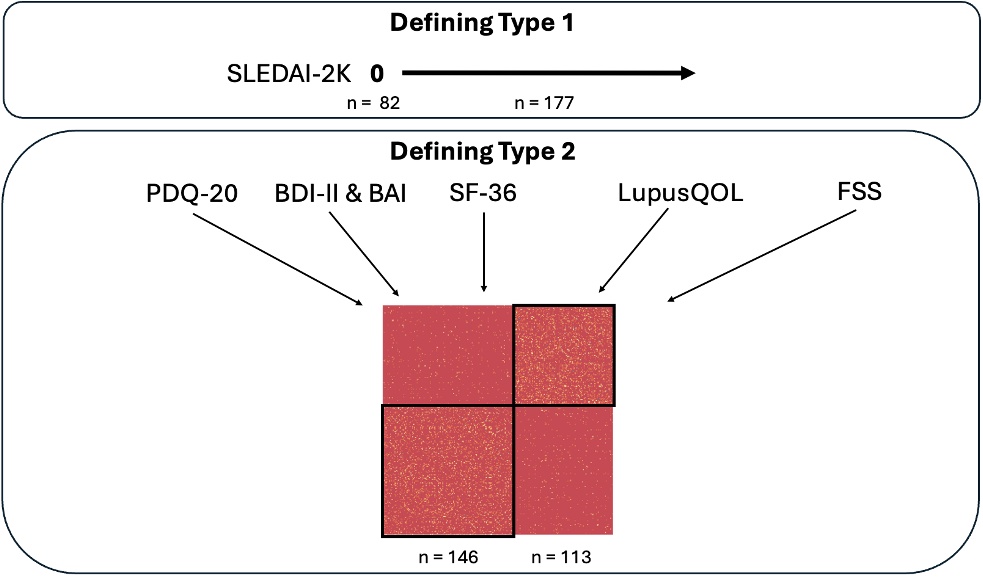
Methods: This was a cross-sectional study of a single cohort of SLE patients who participated in a trial studying cognitive impairment and recruited prospectively since 2016. Type 1 activity was defined as a clinical SLEDAI-2K of >0 (excluding C3, C4 dsDNA levels). As there is no clear definition of Type 2 activity, we aimed to define this based on different PRO measures: Beck Depression and Anxiety Inventories (BDI-II and BAI), Lupus Quality of Life (Lupus QoL), Fatigue Severity Score (FSS), Perceived Deficits Questionnaire (PDQ-20) for subjective cognitive impairment, Short Form Health Survey (SF-36). We conducted a Similarity Network Fusion (SNF) analysis that used spectral clustering to generate participant subtypes and hypothesized that distinct groups would emerge (Figure 1). For our secondary aim, we included variables such as patient characteristics, SLICC/ACR damage index (SDI), antibodies, medications.
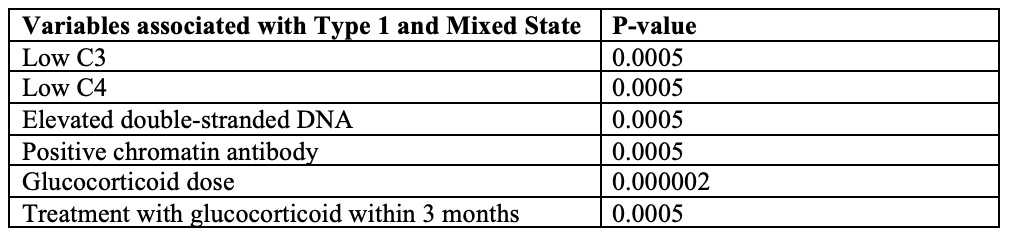
Results: 259 patients were included in the final analysis. Four distinct patient phenotypes emerged: Minimal (32 patients; 12.4%), High Type 1 (81 patients; 31.3%), High Type 2 (50 patients; 19.3%), and Mixed (96 patients; 37.1%). Patients with High Type 2 state had poorer median PRO scores in all measured outcomes (all p-values significant to < 0.0001): PDQ20 (39.5 vs 20), BDI (20.2 vs 6.2), BAI (21 vs 6), SF-36 Mental Component Summary (36.5 vs 54.8) and SF-36 Physical Component Summary (32.2 vs 51.2), FSS (5.56 vs 3.11) and all Lupus QoL domains. Statistically significant variables (p< 0.05 after Bonferroni correction) differentiating the four states included low C3/C4, elevated dsDNA, chromatin antibody presence, glucocorticoid dose and treatment with glucocorticoids within 3 months. The presence of these variables was associated with a High Type 1 and Mixed state (Table 1).
Conclusion: We identified that patients may be categorized into disease states based on Type 1 and Type 2 characteristics – Minimal 13%, High Type 1 31%, High Type 2 19% and Mixed 37%. High Type 2 patients uniformly scored poorly in all PRO domains. Multiple laboratory markers (low C3/4, elevated dsDNA, presence of chromatin antibody) as well as glucocorticoid use were found to predict High Type 1 or Mixed states.
PDQ_20: Perceived Deficits Questionnaire
BDI-II: Beck Depression Inventory
BAI: Beck Anxiety Inventory
FSS: Fatigue Severity Score
SF_36: Short Form Health Survey
LupusQoL: Lupus Quality of Life
To cite this abstract in AMA style:
Hu A, Erdman L, Bonilla D, Li Q, Whittall Garcia L, Gladman D, Touma Z. Characterizing SLE Patients into Type 1 and Type 2 Disease States: Insights from a Single Lupus Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/characterizing-sle-patients-into-type-1-and-type-2-disease-states-insights-from-a-single-lupus-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterizing-sle-patients-into-type-1-and-type-2-disease-states-insights-from-a-single-lupus-cohort/