Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The spread of misinformation related to COVID-19 has been especially acute for SLE patients as unsubstantiated claims regarding the efficacy of antimalarials for COVID-19 first jeopardized drug supplies, and then misinformation regarding toxicity provoked abrupt discontinuation. Conflicting health messages based on unfounded information can contribute to detrimental health decisions, exacerbate stress, and precipitate SLE flares. In attempt to mitigate the adverse consequences of accessing, spreading, and acting on misinformation, we assessed how SLE patients access health information pre and during COVID-19.
Methods: SLE patients fulfilling the ACR or Systemic Lupus International Collaborating Clinics (SLICC) Classification Criteria for SLE from a patient cohort in Alberta, Canada completed an online survey in June 2020 regarding the sources of health information they accessed in the 12 months preceding (pre March 11, 2020) and during the COVID-19 (post March 11, 2020) pandemic. Descriptive statistics were used to calculate the percentage of patients accessing each source of information, their preferred sources, and the level of trust in each source. McNemar tests were used to compare frequencies preceding and during the pandemic.
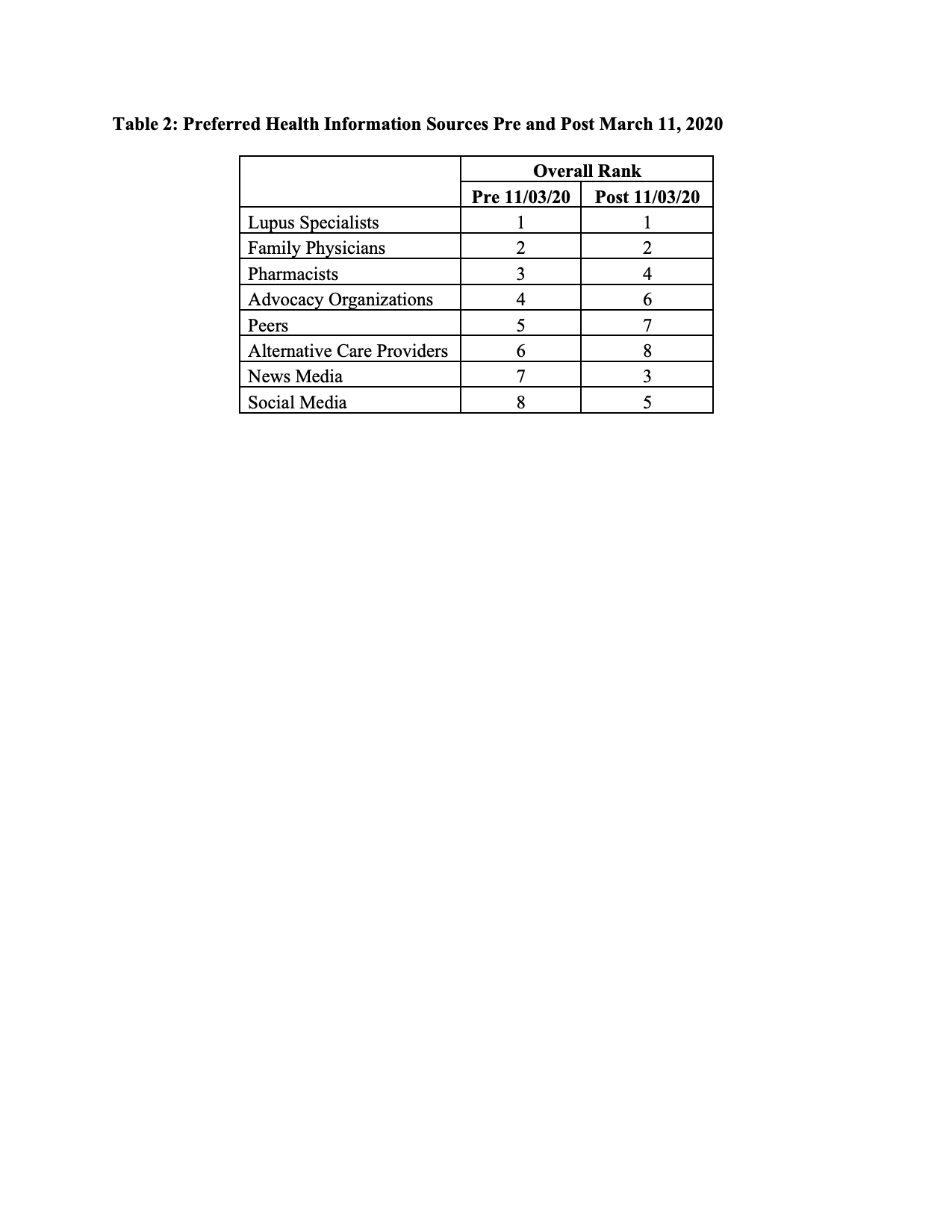
Results: 106 of 248 patients completed the survey (43% response rate); 91.5% were female, 71.7% Caucasian, and the mean age at diagnosis was 35.9 years (SD 14.0) and mean disease duration was 16.6 years (SD 12.8). 73.6% had completed some form of post-secondary education, and 83% reported taking antimalarials in the past 12 months. No participants reported a doctor diagnosis of COVID-19. Patients accessed news media more frequently during the pandemic (38.7% accessed sometimes/often/always pre vs 56.6% post), while access to family physicians, SLE specialists, pharmacists and alternative care providers decreased during the pandemic (Table 1). Lupus specialists and family physicians were ranked the most preferred (Table 2) and considered the most trustworthy sources (Table 3) pre and during the pandemic. News and social media were ranked more highly as preferred sources post vs pre March 11 (Table 2), but were considered much less trustworthy than physicians (86.8% rated lupus specialists as somewhat/very trustworthy post vs 38.7% for online news media).
Conclusion: Although SLE specialists and family physicians are ranked as the most preferred and trustworthy sources of health information, patients accessed these sources less frequently during the pandemic and accessed news media, a less preferred source, more frequently. This study is currently being expanded to include additional Canadian and international centers to further investigate the sociodemographic and geographic factors influencing access to and use of health information. This research will improve existing information dissemination pathways valued by SLE patients and enhance public health response during the pandemic and beyond.
To cite this abstract in AMA style:
Cardwell F, Elliott S, Choi M, Chin R, Clarke A. Characterizing How SLE Patients Access Health Information Pre and During COVID-19 [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/characterizing-how-sle-patients-access-health-information-pre-and-during-covid-19/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterizing-how-sle-patients-access-health-information-pre-and-during-covid-19/