Session Information
Date: Monday, November 8, 2021
Title: Epidemiology & Public Health Poster III: Other Rheumatic & Musculoskeletal Diseases (1022–1060)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: This study evaluated the patterns of care, access and direct costs related to the management and treatment of patients with systemic lupus erythematosus (SLE) in Brazil.
Methods: This cross-sectional study (GSK Study 207353) assessed patients ≥18 years of age with SLE (ACR, 1997 classification criteria) who had been receiving SLE care for ≥1 year at 5 SLE reference facilities. The study period was 12 months. Patients retired or on leave owing to another illness were excluded. Clinical information and resources used in clinical practice were obtained by interviewing patients and medical records. Direct resources were categorized as: (1) health-related hospital resources: consultations, tests, medications, hospitalization; (2) non–health-related hospital resources: transportation, home adaptation, spending on caregivers. The drugs were categorized as: (1) specific for SLE, according to coverage by the Brazilian public system; (2) adjuvants, used in the management of comorbidities. Costs were calculated at the unit value of each resource in relation to the quantity consumed. A multivariate regression model sought to explore cost predictors in this group of patients.1
Results: Three hundred patients with SLE (92.3% female, mean [standard deviation, SD] duration of disease of 11.8 [7.9] years) were included. Overall, the time (mean [SD]) between the onset of the first symptoms and the start of treatment was 21.6 (39.6) months (Table 1). Forty-six (15.3%) patients stopped schooling because of the disease and 33.3% were retired or on sick leave because of SLE. Mean (SD) travel time from home to a care facility was 4.4 (12.6) hours. Antimalarials were the drugs most used by patients (n=222 [74.0%]) followed by mycophenolate mofetil (n=90 [30.0%]). The mean total cost for SLE in Brazil was US$3123.53 per patient per year (median [interquartile range, IQR] US$1618.51 [678.66; 4601.29]). The main item that contributed to the expenditure was medication, with a median (IQR) cost of US$910.62 (460; 4033.51), followed by hospitalization (US$900.60 [382.10; 2,106.41]; Table 2). According to the regression model, mycophenolate use increased the cost by 3.664 times (p< 0.001). Also, inflammatory monitoring (erythrocyte sedimentation rate [ESR] or C-reactive protein) reduced expenditure by 0.381 times (p< 0.001; Table 3).
Conclusion: The cost of SLE in Brazil is driven by the use of immunosuppressants or by its frequent monitoring, and hospitalization.
Funding: GSK
References:
1de Abreu MM, et al. Perit Dial Int 2013;33(3):304–15
2Brazilian health information system. Available from: http://www2.datasus.gov.br/datasus/index.php?area=02. [last accessed February 12, 2021]
3Agência Nacional de Vigilância Sanitária (ANVISA). Available from: https://www.gov.br/anvisa/pt-br/assuntos/medicamentos/cmed/compras-publicas/lista-de-precos-maximos-para-compras-publicas. [last accessed February 12, 2021]
 Table 1. Distribution of sociodemographic characteristics, clinical classification and treatment for patients with SLE
Table 1. Distribution of sociodemographic characteristics, clinical classification and treatment for patients with SLE
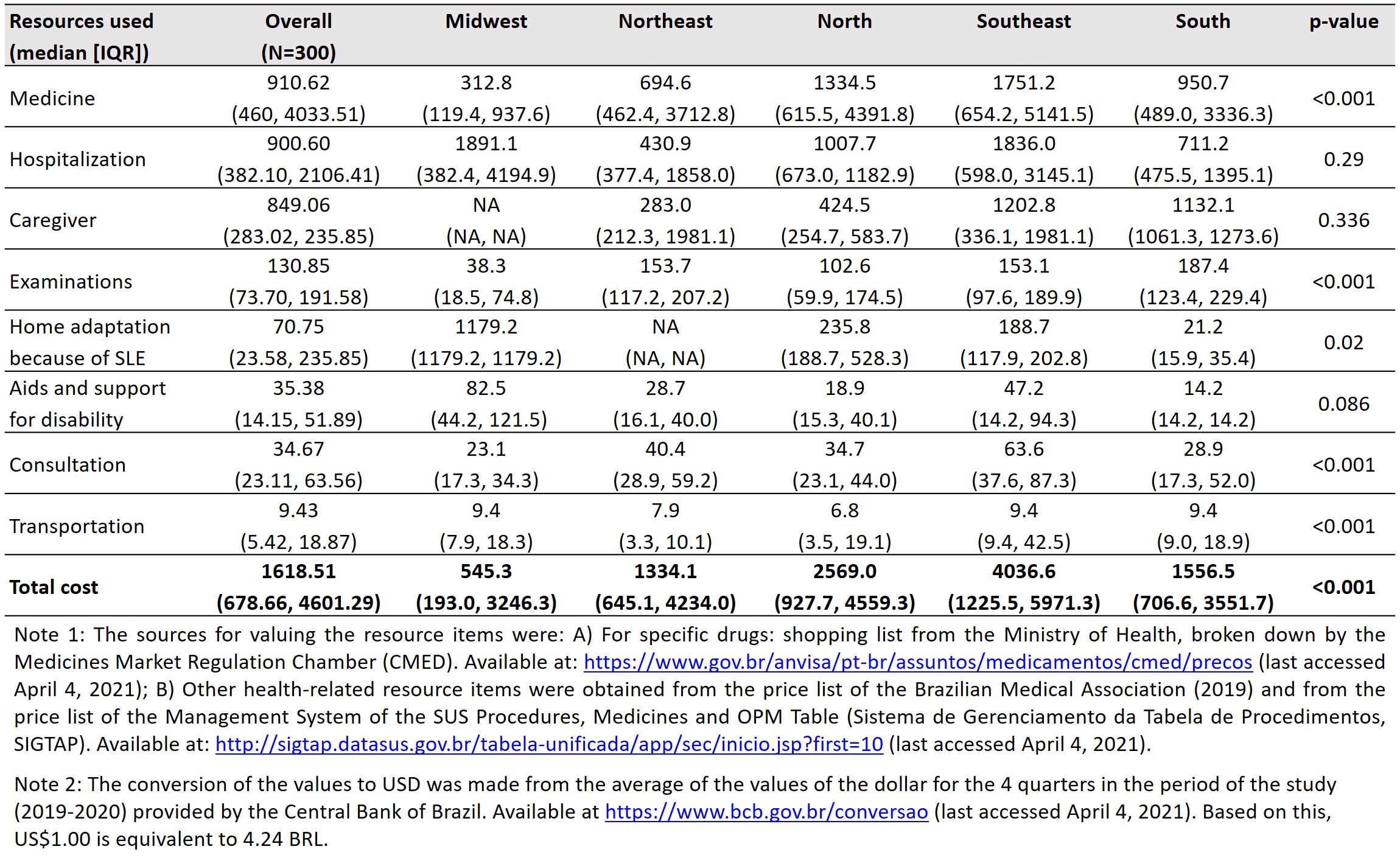 Table 2. Distribution of the cost of SLE, per patient per year, according to geographic region and type of resource consumed, in US$ [2,3]
Table 2. Distribution of the cost of SLE, per patient per year, according to geographic region and type of resource consumed, in US$ [2,3]
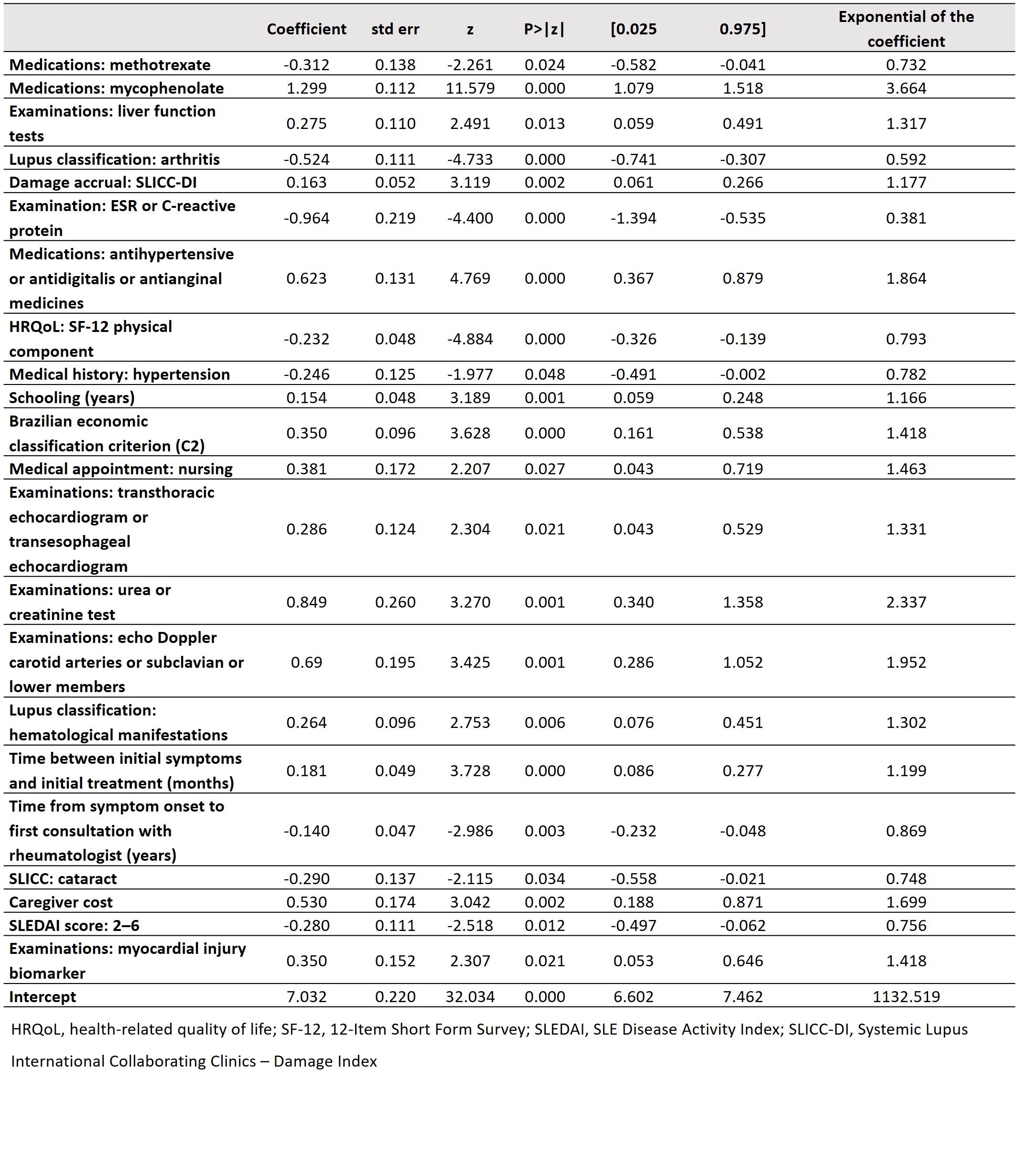 Table 3. Multivariate regression model to assess the factors that influence the total cost per patient per year
Table 3. Multivariate regression model to assess the factors that influence the total cost per patient per year
To cite this abstract in AMA style:
Mendes de Abreu M, Fernandes V, Andre Monticielo O, Cristovão Maiorano A, dos Santos Beserra F, Rachel Moreira Lamarão F, David N, de Veras B, Araujo M, Elena Rios Gomes Bica B, Luise Andrade Souto Rodrigues D, Andrade Bulbol G, Jardim Martins da Silva N, Sávio Nunes de Lima D, Maria das Chagas Medeiros M. Characterization of the Patterns of Care, Access and Direct Costs of Systemic Lupus Erythematosus in Brazil: Findings from the Macunaíma Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/characterization-of-the-patterns-of-care-access-and-direct-costs-of-systemic-lupus-erythematosus-in-brazil-findings-from-the-macunaima-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterization-of-the-patterns-of-care-access-and-direct-costs-of-systemic-lupus-erythematosus-in-brazil-findings-from-the-macunaima-study/
