Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Positive antinuclear antibodies (ANAs) cause diagnostic dilemmas for clinicians across specialties. We previously developed and validated a risk model to predict risk of developing systemic autoimmune disease in positive ANA patients. We have deployed this risk model in real-time in the electronic health record (EHR) and examine patient and provider factors in these positive ANA patients.
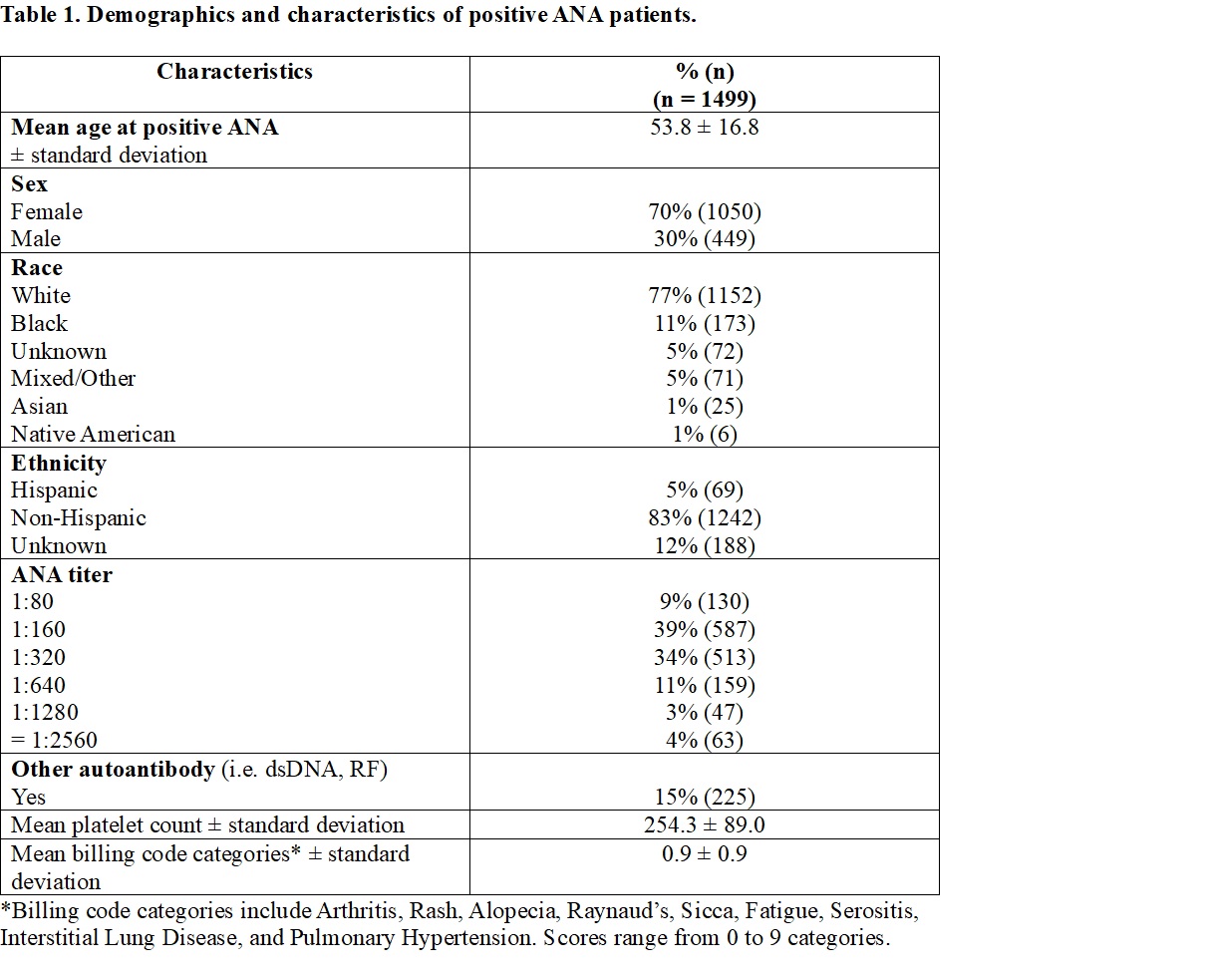
Methods: We identified all positive ANA patients (≥ 1:80) from July 2023 to May 2024 at Vanderbilt University Medical Center (VUMC). A priori, we excluded patients who were ≤ 18 years old, admitted at time of positive ANA, previously seen by rheumatology, and had a prior positive ANA at VUMC to capture adult, incident, and outpatient positive ANA patients. We calculated a risk score for developing autoimmune disease using our published logistic regression model that includes age at first positive ANA, sex, ANA titer, platelet count, billing codes for symptoms of autoimmune diseases, and presence of another autoantibody (i.e. dsDNA). We examined the above patient factors, race, ethnicity, and ordering provider training and specialty.
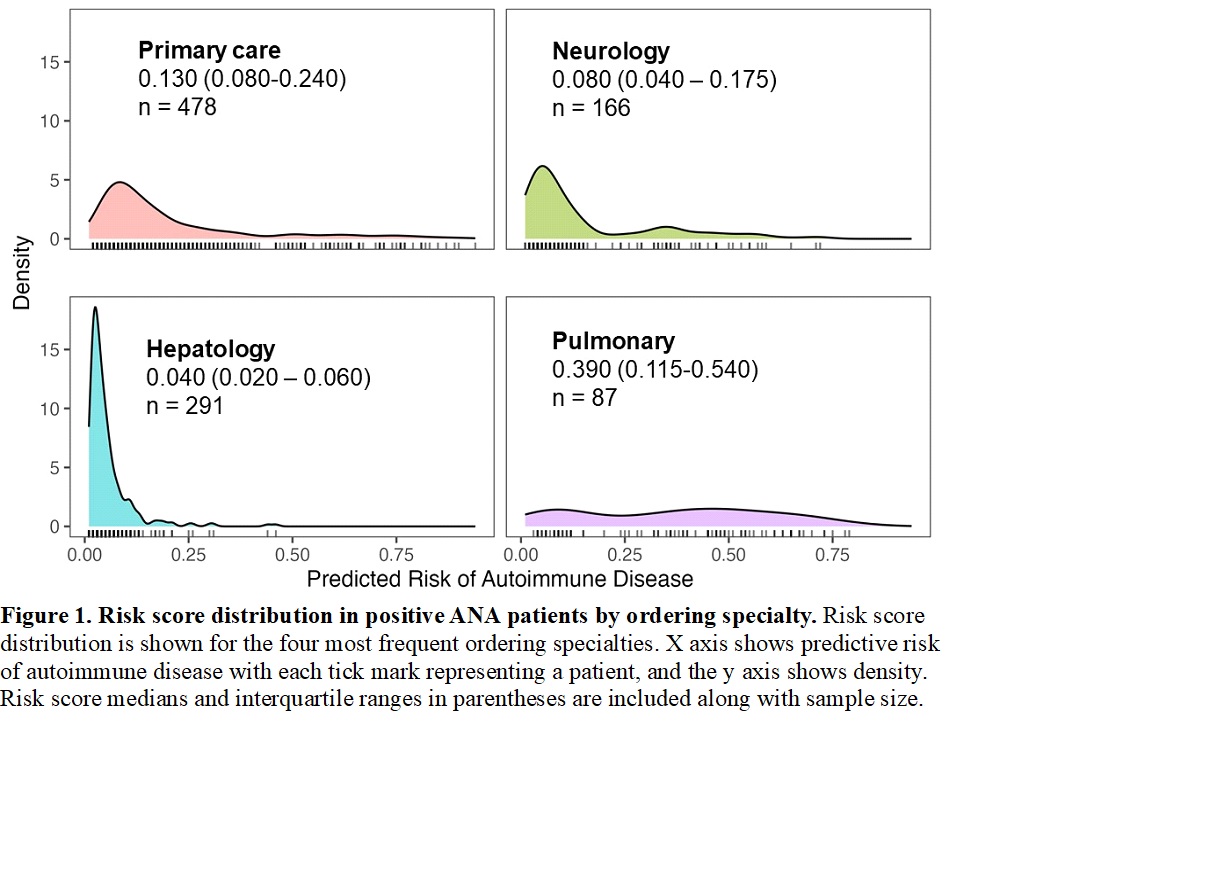
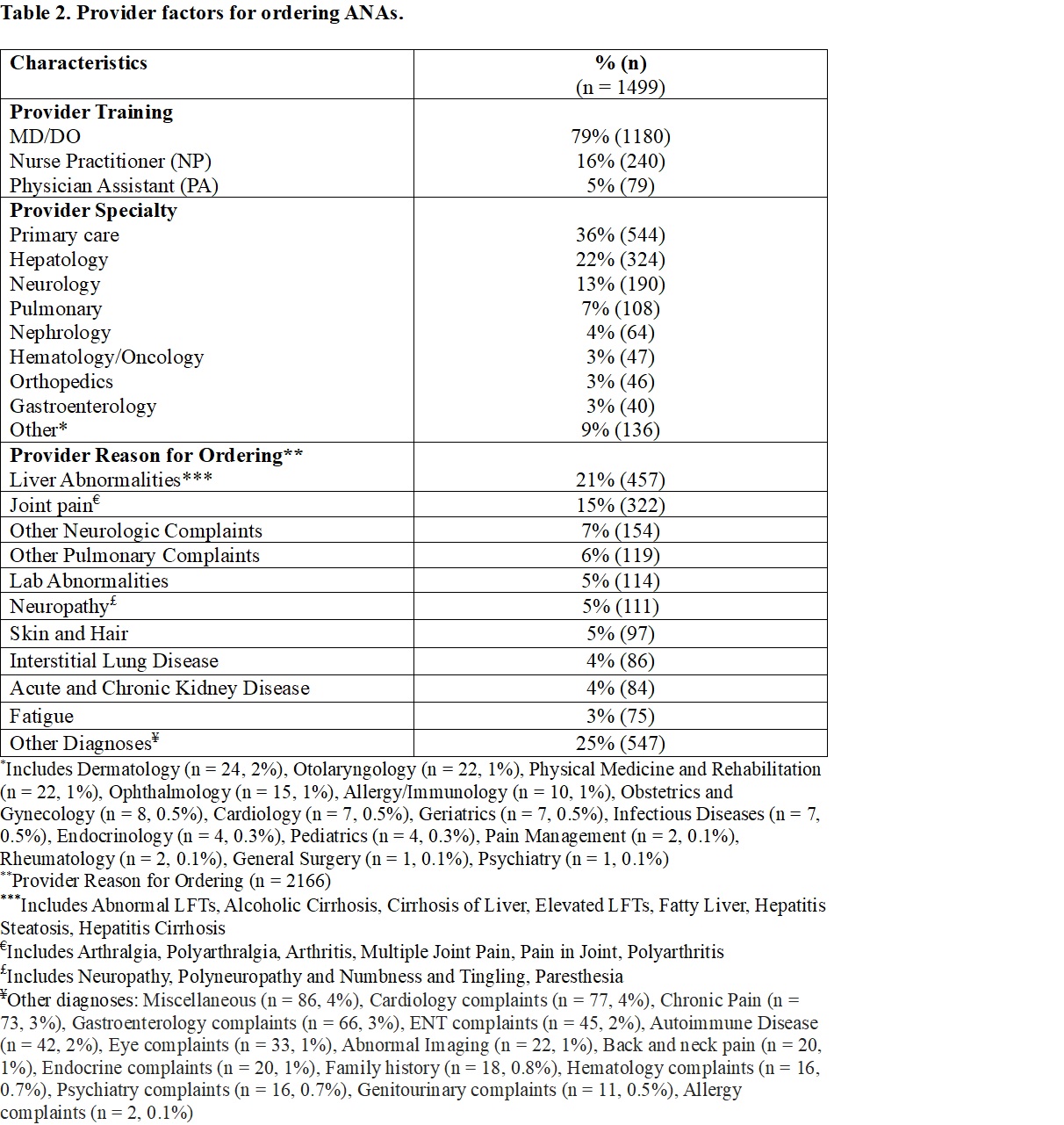
Results: We included 1499 patients with positive ANAs who are 70% female, 30% male, and have a mean age at ANA ordering of 53.8 ± 16.8 years (Table 1). Of these patients, 77% were White, 11% Black, 5% Other, and 5% Hispanic. Most patients had a positive ANA of 1:160 (39%) or 1:320 (34%) with 15% having another autoantibody. MD/DOs were more likely to order an ANA than NP/PAs (79% vs. 21%, p < 0.001) (Table 2). The most frequent ordering specialties were primary care (36%), hepatology (22%), neurology (13%), and pulmonary (7%). There were 2166 distinct billing codes used for ordering ANAs. The most frequent were liver abnormalities (n = 457, 21%), joint pain (n = 322, 15%), and neurologic complaints (n = 154, 7%). For primary care, the most frequent reasons were joint pain, fatigue, and myalgia. For hepatology, it was almost exclusively liver abnormalities, and for neurology, neuropathy and paresthesia. Lastly, for pulmonary, it was interstitial lung disease (ILD) and pulmonary hypertension (PH). Risk scores for developing autoimmune disease based on the most frequent ordering specialties are shown in Figure 1. Median risk scores were higher for pulmonary (0.390) [IQR: 0.115-0.540] compared to primary care (0.130) [IQR:0.080-0.240], hepatology (0.040) [IQR:0.020-0.060], and neurology (0.080) [IQR: 0.040-0.175] (p < 0.001).
Conclusion: We demonstrate ANA ordering most commonly by primary care. ANA ordering is most frequently requested due to joint pain but also for non-specific symptoms such as fatigue and myalgia. Risk scores were low for patients who had ANAs ordered by the most frequent ordering specialties. Risk scores were higher for patients who had ANAs ordered by pulmonary, likely capturing patients with connective tissue disease related ILD and PH. Frequent positive ANA referrals occur in the setting of a rheumatology workforce shortage. Triaging positive ANA referrals is important to ensure high-risk patients are seen for timely diagnoses while reducing unnecessary referrals for low-risk patients.
To cite this abstract in AMA style:
Grace E, Green S, Nikolova N, Suh A, Moore R, Domenico H, McCoy A, Barnado A. Characteristics of Ordering Providers and Patients with Positive Antinuclear Antibodies: A Pragmatic, Risk Model Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/characteristics-of-ordering-providers-and-patients-with-positive-antinuclear-antibodies-a-pragmatic-risk-model-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-of-ordering-providers-and-patients-with-positive-antinuclear-antibodies-a-pragmatic-risk-model-study/