Session Information
Date: Tuesday, October 28, 2025
Title: (2015–2051) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile idiopathic arthritis (JIA) is the most common chronic rheumatic disease in childhood. Up to one-third of patients experience disease flares in adulthood, with significant clinical and therapeutic implications. The introduction of biologic therapies in the year 2000 marked a paradigm shift in managing these patients, leading to better disease control and reduced long-term sequelae. However, limited data are available on how patient characteristics at diagnosis, particularly across different periods, influence disease progression and therapeutic management.
Methods: Retrospective, cross-sectional study including patients diagnosed with JIA between 1960 and 2024 who had at least one follow-up visit in an adult rheumatology clinic at a tertiary care hospital. Sociodemographic, clinical, and laboratory data were collected. Patients with systemic JIA were excluded due to their distinct clinical characteristics.
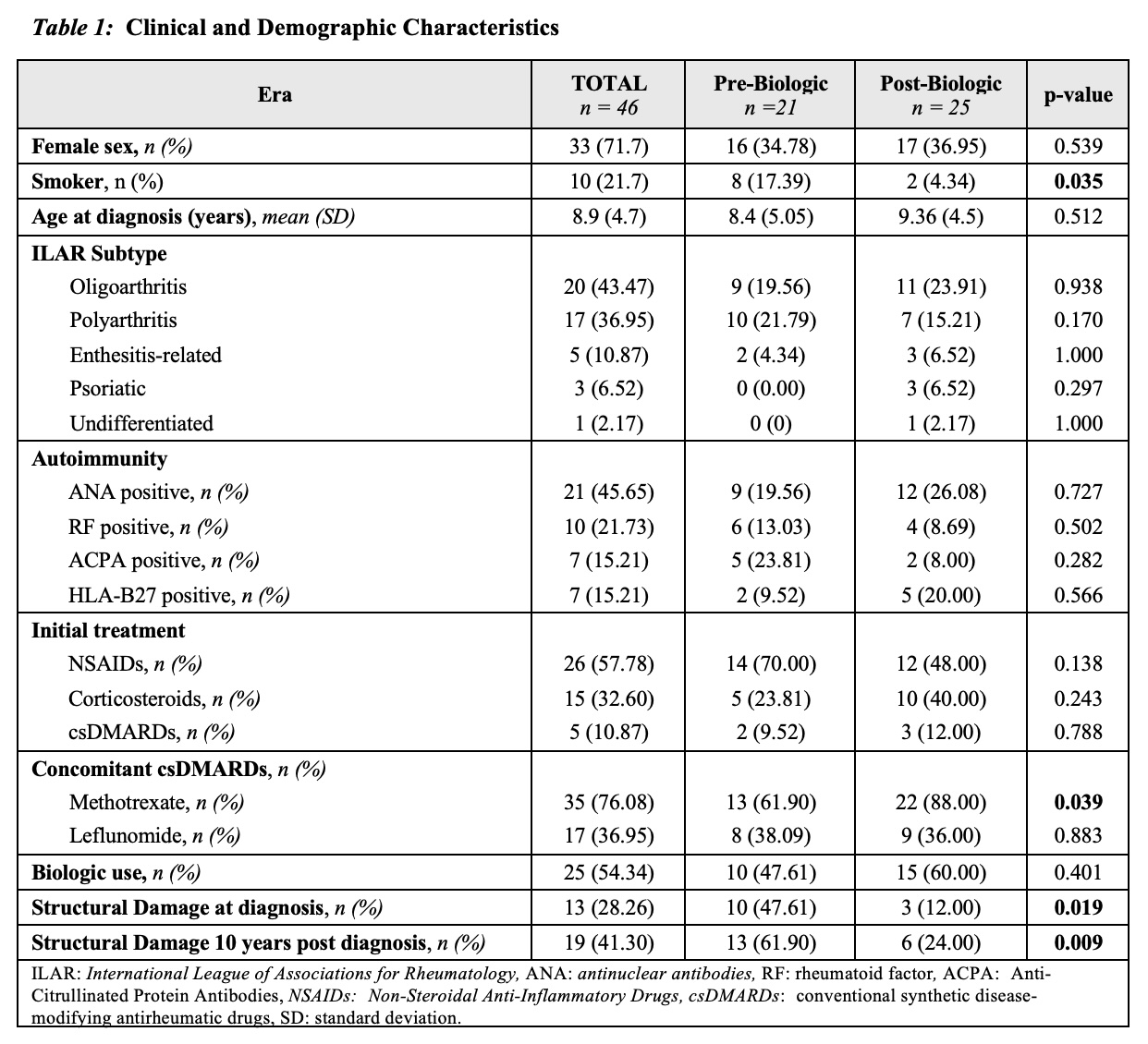
Results: A total of 46 patients were included (Table 1), predominantly female (71%), with a mean age at diagnosis of 8.9 ± 4.7 years, slightly higher in patients diagnosed after 2000 (9.36 ± 4.5 years). No significant differences were found regarding disease subtypes or autoimmune markers between patients diagnosed in the pre-biologic era (n=21) and post-biologic era (n=25).The first-line treatment in 58% of cases was NSAIDs, followed by corticosteroids (32%). Among post-2000 patients, 88% required concomitant methotrexate treatment. Biologic therapy was required at some point in the disease course in 60% of post-biologic era patients, compared to 47% in the pre-biologic group (p=0.401). Disease duration and age at initiation of the first biologic were significantly higher in the pre-biologic group (28.4 ± 12.65 years and 37.4 ± 15.38 years) compared to the post-biologic group (6.4 ± 5.71 years and 16.7 ± 4.77 years) (p < 0.001 for both).Structural joint damage at baseline and after 10 years of treatment was significantly greater in the pre-biologic group than in the post-biologic group (p = 0.019). Among all patients who received biologic therapy, 96% were initially treated with anti-TNF agents, with etanercept being the most used (56%).
Conclusion: In our cohort, patients diagnosed with JIA in the pre-biologic era had significantly greater initial structural damage than those diagnosed in the post-biologic era, possibly due to delayed diagnosis. Furthermore, the longer disease duration before initiation of biologic therapy and older age at first biologic use observed in the pre-biologic group may have contributed to increased long-term joint damage, highlighting the potential impact of earlier biologic intervention.
To cite this abstract in AMA style:
salabert-Carreras F, Ugena-García R, Rocamora-Gisbert C, Calomarde-Gómez C, Churtichaga Domenech C, Vidal ripoll J, MATEO SORIA L, Gifre-Sala L, Aparicio M, Holgado S, Prior Español Á, Riveros frutos A, Casafont-Solé I, Forcadell Pirretas E, Pujol Manresa A, Font-Urgelles J, Martínez-Morillo M, Nack A. Characteristics of a Historical Cohort of Adult Patients with Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/characteristics-of-a-historical-cohort-of-adult-patients-with-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-of-a-historical-cohort-of-adult-patients-with-juvenile-idiopathic-arthritis/