Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose:
Healthy ageing and the occurrence of the common age-related disease osteoarthritis (OA) result from varying degrees of interaction between many determinants (genetic, lifestyle). Immuno-senescence and inflammageing are features of the ageing immune system. Age-related abnormalities (loss of T-cell reactivity, development of autoantibodies, activation of inflammatory mechanisms) may be synergising with structural defects of the musculoskeletal system aiding the development of OA. We aimed to determine if abnormalities of blood immune cell composition are associated with OA, beyond the defects already associated with age.
Methods:
Blood samples were collected from 120 healthy controls (age range 18-69) to establish variations associated with age and 120 OA (age range 49-80). We examined loss or acquisition of age-related changes in blood composition. 8-colours flowcytometry was performed to establish the frequencies of: CD4/CD8, B, NK-cells. Naïve and regulatory T and B-cell were subsequently analysed and cells with an abnormal phenotype identified in Rheumatoid arthritis is direct relation with inflammation (IRC phenotype).
Results:
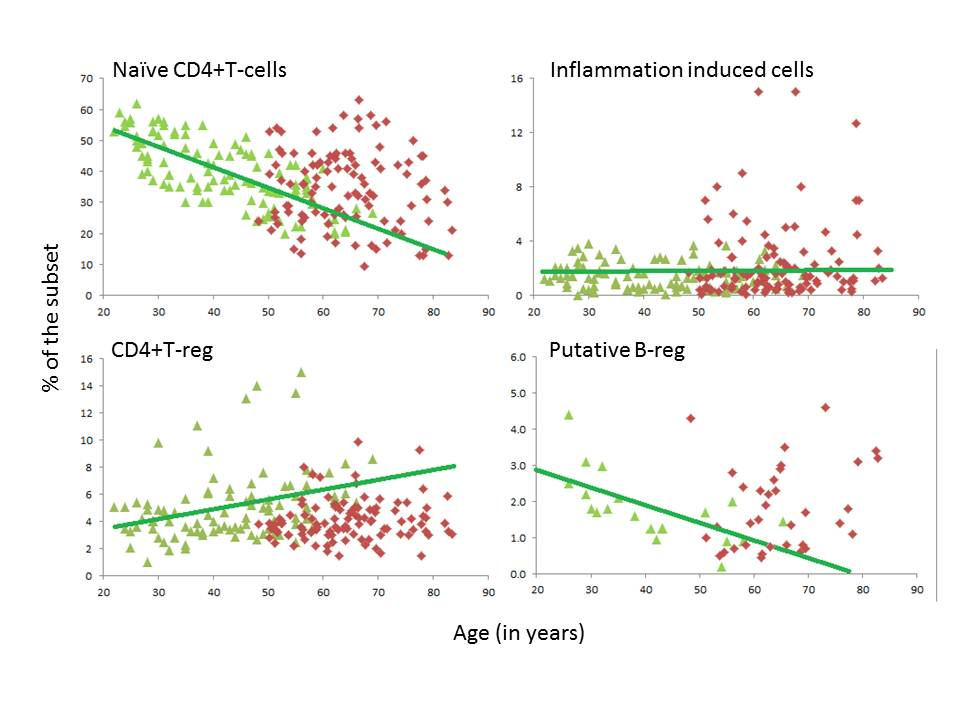
Flowcytometry was performed on all 240 samples (only 20 HC and 45 OA were analysed for B-cells) and demonstrated, as expected, very little change in lineage representation associated with age in health with: no change for NK, CD4, and B-cells, weak decline in CD8 (rho=-0.300, p=0.019) and increase in NKT (rho=0.315, p=0.012). In contrast phenotyping T and B-cells showed clear age-related changes with reduction of naïve CD4 T-cell (rho=0.817, p<0.0001). Regulatory T-cells increased (rho=0.401, p<0.0001) whereas B-reg reduced (rho= -0.658, p=0.002). IRC were not related to age.
In OA differences were observed. NK, CD4 and B cells were not related to age but in OA, NK cells were positively correlated (rho=0.350, p<0.0001), CD4 (rho=-0.318, P=0.001) and B-cells (rho=-0.260, p=0.006) negatively. The NKT correlation with age was maintained in OA (rho=0.296, p=0.002) but the CD8 relationship was lost. Naïve CD4 cells appeared to be particularly affected (see Figure 1 showing % of several subsets) with considerable increase in frequency. Treg were reduced in most patients irrespective of age. B-cell subsets were not particularly affected although the age-relationship for B-reg was lost. IRC were not increased with the exception of ~20 patients.
Conclusion:
This analysis of the immune cell composition of the blood of OA patients suggests that immune dysfunction is present in OA above what is directly related to ageing. Immuno-senescence and inflammageing (as suggested by the increased frequency of IRC in some OA patents) may therefore play a role in OA in addition to their implication in healthy ageing.
Figure 1. Cell subsets % in OA and HC ( HC-green triangles, OA red diamonds)
Disclosure:
A. Burska,
None;
M. Campbel,
None;
R. Raja,
None;
D. White,
None;
P. Emery,
None;
P. G. Conaghan,
None;
F. Ponchel,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/changes-in-peripheral-blood-immune-cell-composition-in-osteoarthritis/