Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
RA patients are managed using treat-to target (T2T) regimens often utilizing the DAS28CRP as an outcome measure. In this study we compared clinical changes in RA disease activity with changes in MRI inflammation on T2T escalation.
Methods:
80 seropositive rheumatoid arthritis (RA) patients on conventional disease-modifying anti-rheumatic drugs (cDMARDs) were enrolled if they had DAS28CRP > 3.2: Group A escalated to another cDMARD combination, Group B to anti-TNF therapy/cDMARDs. Contrast-enhanced 3T-MRI wrist scans were obtained before (V1) and 4 months after (V2) regimen change. Scan pairs were scored by one experienced radiologist reader for synovitis, osteitis and tenosynovitis, summed as MRI inflammation (MRI(i)) score, plus erosions. Associations between DAS28CRP and MRIi were investigated.
Results:
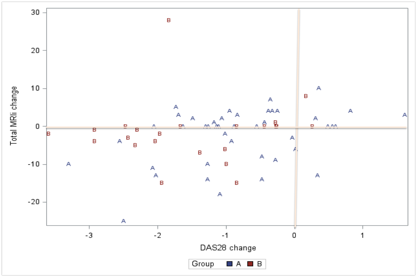
58 patients were enrolled in Group A (42 female, 16 male) and 22 in Group B (18, 4). 66 scan pairs were available for analysis including 8 pairs from 4 patients who were sequentially enrolled into Group A then Group B. Intra-reader reliability was high: ICC(av) 0.89 (0.56 – 0.97). DAS28CRP and disease duration (months) were lower in Group A than B; 4.22 vs 5.16 (p = 0.001) and 30 vs 77 (p = 0.01). Change in DAS28CRP (median (range) Group A: -0.92 (-3.30, 1.61), Group B: -1.38 (-3.59, 0.26) (p =0.31). Change in MRI(i) Group A, 0 (-25, 7) and Group B, 0 (-7, 28) (p =0.37). Combining groups, change in MRI(i) correlated with change in DAS28CRP (SpearmanÕs 0.36, P = 0.003). Using multiple linear regression analysis adjusting for age, gender, duration, anti-CCP titer and MRI erosion score (V1), change in DAS28CRP was associated with change in MRI(i) so that for every unit increase in change in DAS28CRP there was a 1.83U increase in change in MRI(i), p = 0.052. The components of MRI(i) were analyzed and only MRI tendonitis correlated with change in DAS28CRP (SpearmanÕs 0.33, P = 0.007). There was no significant difference between groups for change in MRI(i) although the fall in score was numerically greater for Group A (- 3.61) than Group B (- 0.73) , p = 0.18. Change in MRI(i) was associated with the MRI erosion score (V1) (p = 0.0054).
Conclusion:
We report the first study investigating the link between clinical and imaging inflammation on T2T escalation in a real world RA cohort. The association was surprisingly weak, especially in those escalating to anti-TNFs where chronic inflammation associated with longer disease duration may have been less amenable to intervention. Given the efficacy of T2T regimens using clinical targets, the use of MRI targets cannot be advocated as yet. Further studies are needed to investigate the long-term implications of persisting MRI inflammation in clinically normal joints.
Figure 1. Change in MRI inflammation score vs change in DAS28CRP on T2T escalation on therapy in Group A and Group B
To cite this abstract in AMA style:
McQueen FM, Chapman PT, Pollock T, D'Souza D, Lee A, Dalbeth N, Stamp LK, Lindsay K, Doyle A. Changes in Clinical Disease Activity Are Associated with Changes in the Total MRI Inflammation Score in Rheumatoid Arthritis Patients Who Are Escalating Therapy in a Treat-to-Target (T2T) Regimen [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/changes-in-clinical-disease-activity-are-associated-with-changes-in-the-total-mri-inflammation-score-in-rheumatoid-arthritis-patients-who-are-escalating-therapy-in-a-treat-to-target-t2t-regime/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/changes-in-clinical-disease-activity-are-associated-with-changes-in-the-total-mri-inflammation-score-in-rheumatoid-arthritis-patients-who-are-escalating-therapy-in-a-treat-to-target-t2t-regime/