Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Despite improvements, patients with ANCA-associated vasculitis (AAV) have a higher risk of death than the general population. Contemporary treatment is associated with high remission rates, but infection, end-stage renal disease (ESRD), and other complications remain common. To identify research priorities, guide study design, and develop interventions to improve survival, comprehensive data on causes and characteristics of death in a real-world, contemporary AAV cohort are needed.
Methods: We identified patients from a multi-center consecutive inception AAV cohort who were diagnosed and died between 2002-2017. Death was ascertained by linkage to the electronic health record and the National Death Index; death certificates were obtained. Two rheumatologists independently reviewed each chart to extract death details; differences were resolved by consensus. Each death was categorized as resulting from active vasculitis, acute ischemic cardiovascular (CV) event, infection, ESRD, cancer, or other. AAV disease status at the time of death was categorized as “induction” (≤ 6 months since treatment initiation), “flare” (increased disease activity within 6 months), or “remission.” We extracted details regarding treatment and place of death. We also determined the sensitivity of a diagnosis of AAV on a death certificate by tabulating the presence of AAV ICD-10 codes (M31.3, M31.7) on any line.
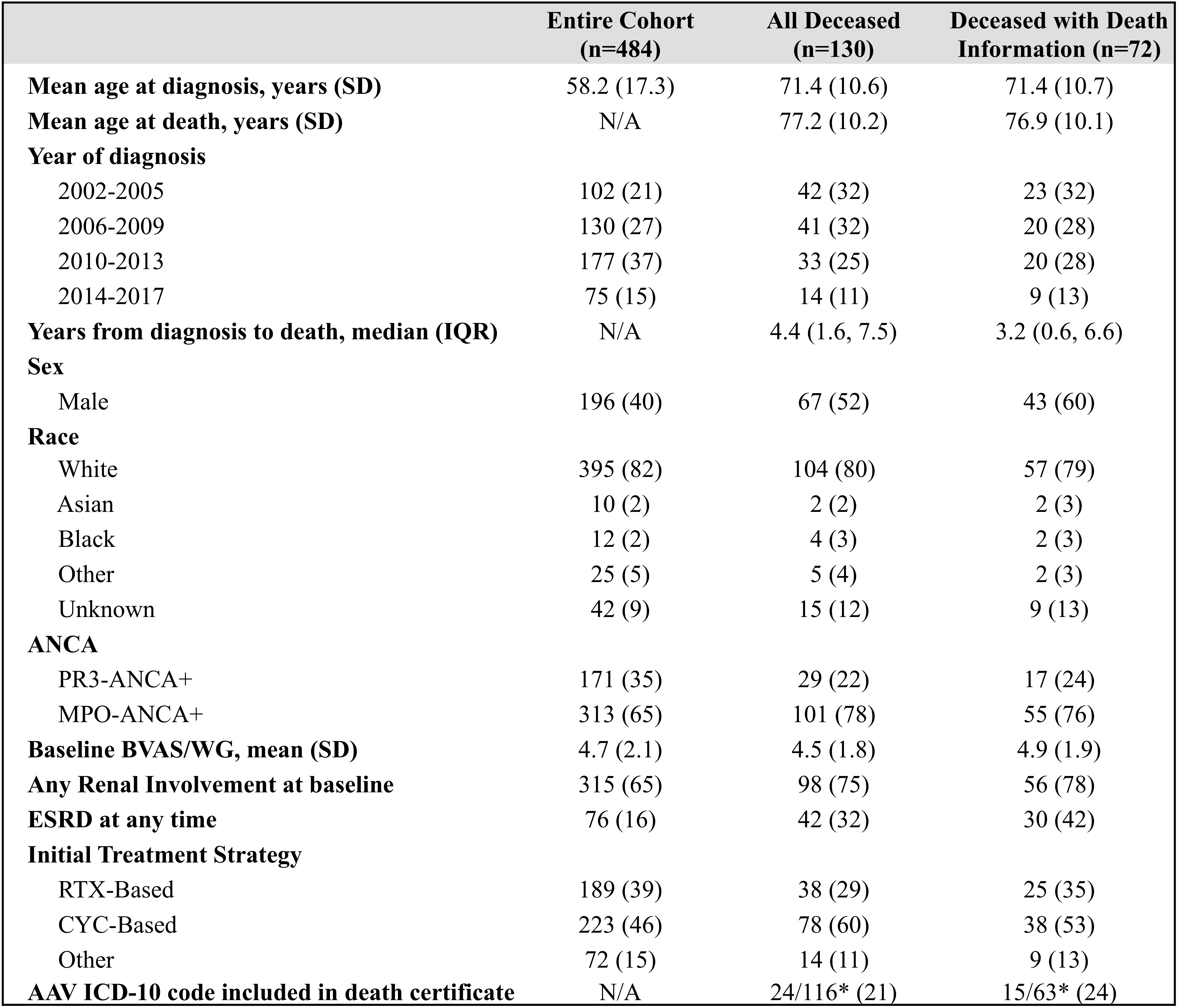
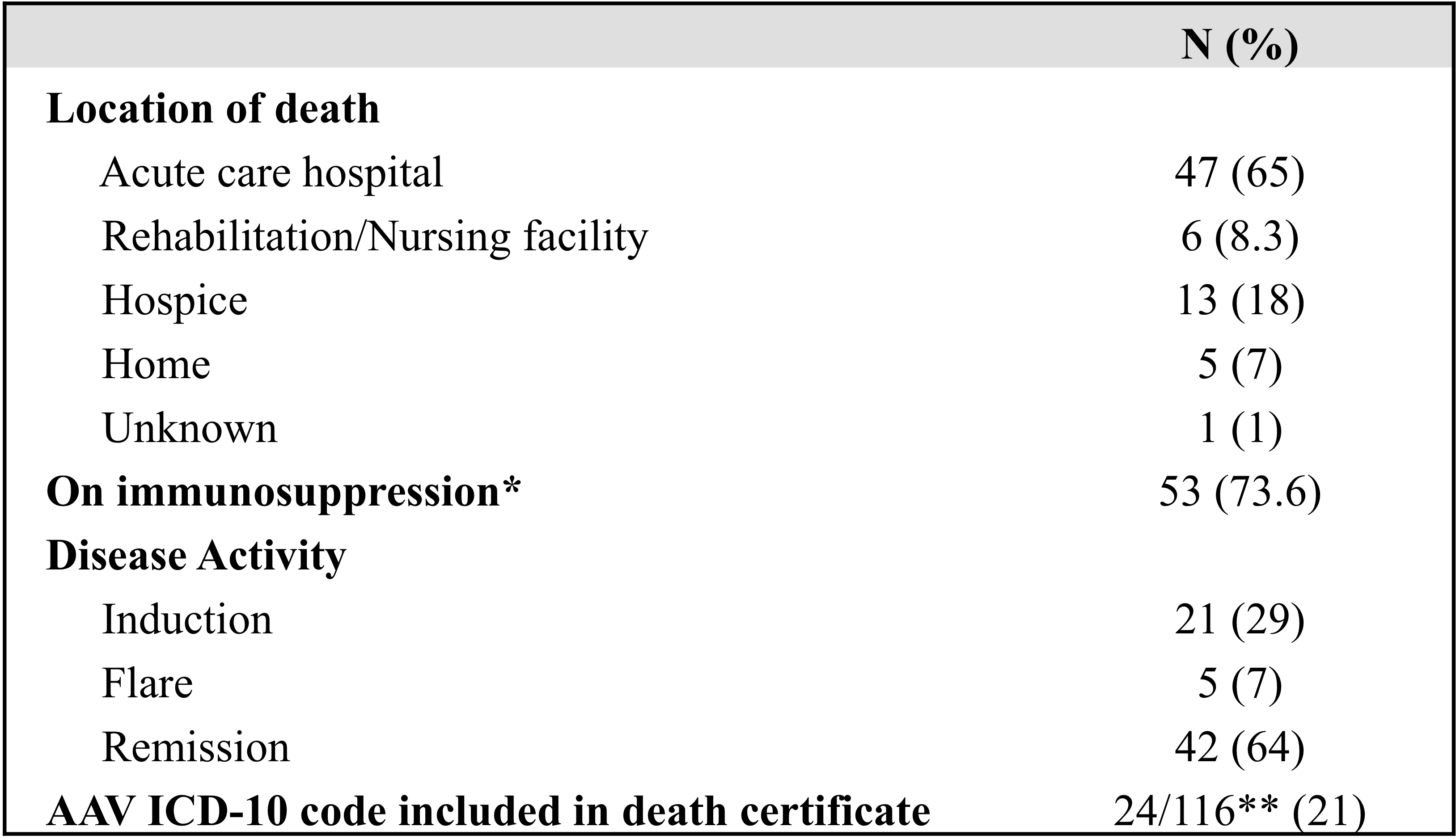
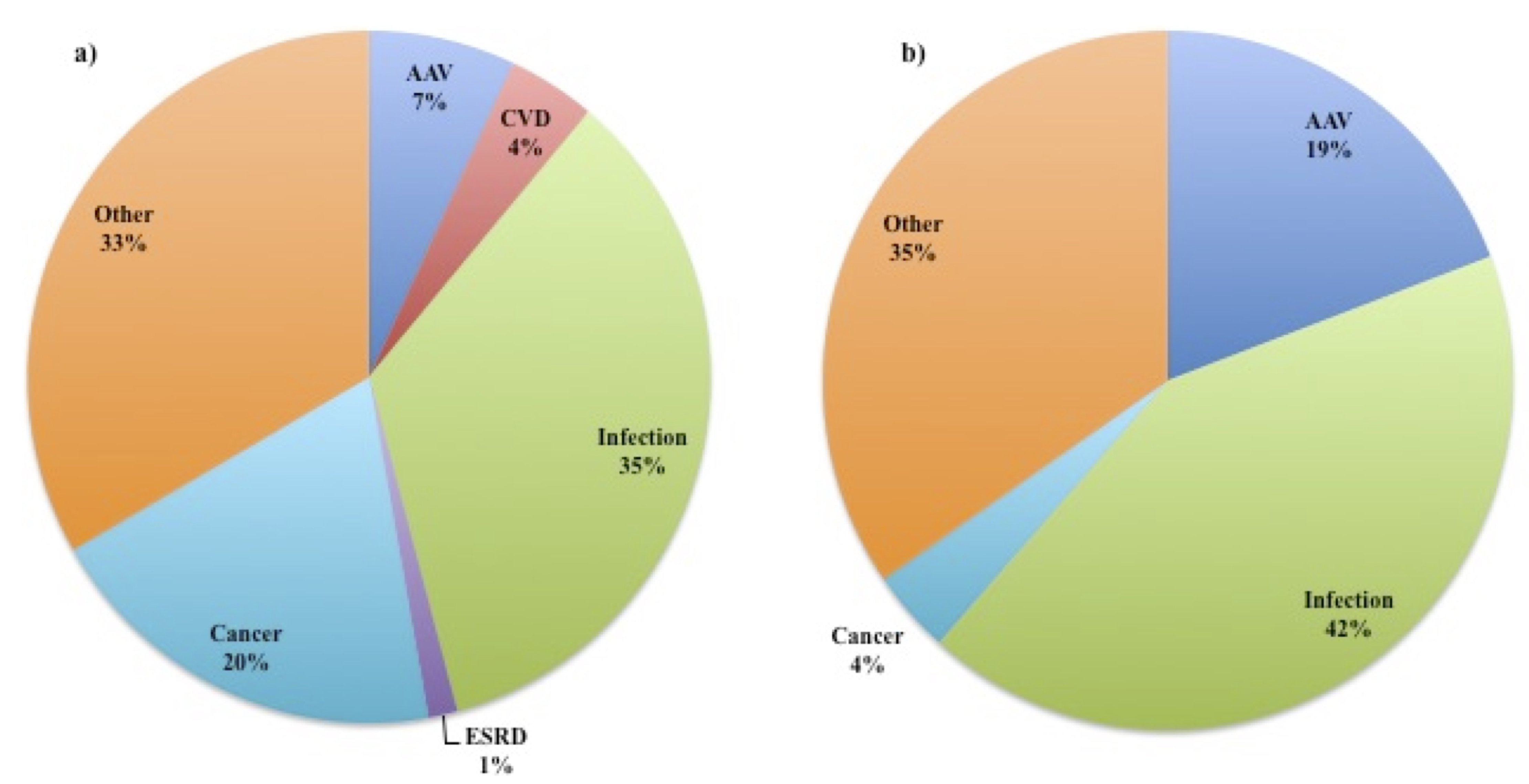
Results: Of 484 patients in the AAV cohort, 130 (27%) died and 72 had records from the time of death available for review. Characteristics of the cohort are included in Table 1. The mean age at death was 71 years, and the median time from diagnosis to death was 4.4 years. 67 out of 130 (52%) were male. Of deaths with EHR data available at the time of death (n=72), 42 (64%) occurred during periods of remission, 21 (29%) during induction, and 5 (7%) during flare. The majority occurred while on immunosuppression (53, 74%), and 47 (65%) occurred in acute care hospitals (Table 2). The most common cause of death was infection (25, 35%), followed by cancer (14, 20%), AAV (5, 7%), acute ischemic CV events (3, 4%), ESRD (1, 1%), and other (24, 33%), which included cardiac arrest of uncertain cause (Figure 1). Deaths from active AAV were rare (5, 7%): cerebral vasculitis (n=1), pulmonary disease (n=3), and multi-organ failure (n=1). Among those with active AAV (induction or flare), infection remained the most common cause (11, 42%). The sensitivity of death certificates for identifying patients with AAV was 21% (24 of 116 certificates); in 3 cases, AAV was misclassified as other vasculitis.
Conclusion: In a contemporary AAV cohort, most deaths were infectious and occurred in remission on maintenance immunosuppression; deaths from active AAV were rare, and some of cardiac etiology were difficult to classify. These results highlight the need for personalized strategies that reduce infection risk during remission maintenance without sacrificing disease control. Additional studies are needed to understand the burden of CV disease in AAV. The use of national death certificate data to estimate the burden of death due to AAV will underestimate the impact of AAV on death.
*Death certificates were not available for 14 patients.
*Treatment with rituximab within the last 6 months or documented B cell depletion at the time of death was considered immunosuppression; other treatments included glucocorticoids and other disease-modifying anti-rheumatic drugs (DMARDs).
**Death certificates were available for 116 patients of total 130 AAV deaths.
To cite this abstract in AMA style:
Katz G, Cook C, Fu X, Choi H, Wallace Z. Causes and Characteristics of Death in ANCA-Associated Vasculitis – A Large, Real-Life, Contemporary Cohort Analysis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/causes-and-characteristics-of-death-in-anca-associated-vasculitis-a-large-real-life-contemporary-cohort-analysis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/causes-and-characteristics-of-death-in-anca-associated-vasculitis-a-large-real-life-contemporary-cohort-analysis/