Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with psoriatic arthritis (PsA) have a higher risk of developing a cardiovascular (CV) event than the general population. This could be attributed to a higher prevalence of traditional CV risk (CVR) factors and to disease characteristics such as systemic inflammation. There are multiple algorithms to estimate the CVR for the general population, however there is not one for PsA patients.
The aim of this study was to compare the CVR reclassification using six CVR algorithms and a carotid ultrasound (US) in PsA patients and controls.
Methods: This was a cross-sectional, observational, and comparative study. A total of 75 patients aged 40-75 years old, who fulfilled the 2006 CASPAR criteria and 75 controls without PsA matched by age (±5 years), gender and comorbidities were recruited for this study. Initially CVR was evaluated according to six CVR algorithms, including Framingham Risk Score (FRS)-lipids, FRS-body mass index (BMI), American College of Cardiology and American Heart Association (ACC/AHA) Risk Algorithm, Systematic Coronary Risk Evaluation (SCORE), QRISK3 and Reynolds Risk Score (RRS). Posteriorly a carotid US was performed in all subjects to identify the presence of subclinical atherosclerosis, defined as the presence of carotid plaque (CP) or an increased carotid intima media thickness (cIMT) which was considered as a value ≥0.8mm. CP was defined as a cIMT ≥1.2mm or a focal narrowing of the surrounding lumen ≥0.5mm. Patients with presence of CP but classified in the low-moderate risk by the CVR algorithms were reclassified to a higher risk category. Distribution was evaluated with the Kolmogorov-Smirnov test. Comparisons were done using χ2 test for qualitative variables, and Student’s t test and Mann-Whitney’s U test for quantitative variables. A p-value < 0.05 was considered statistically significant.
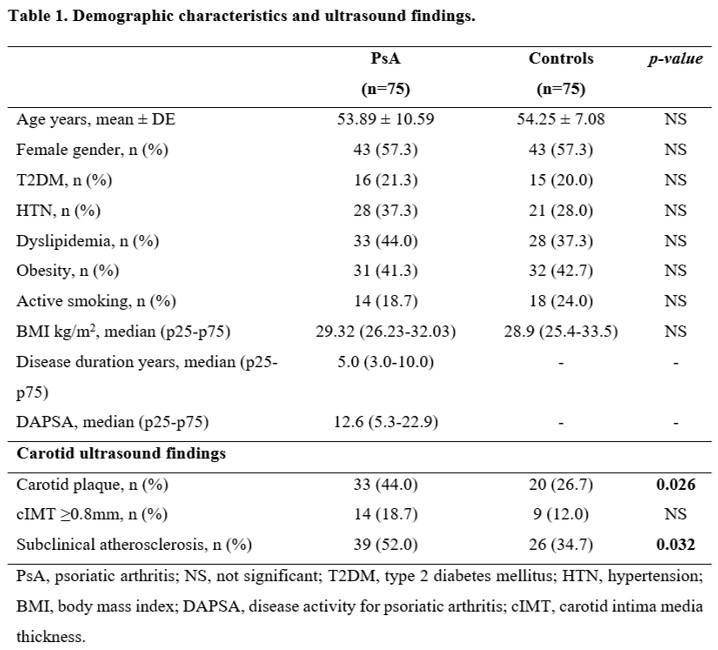
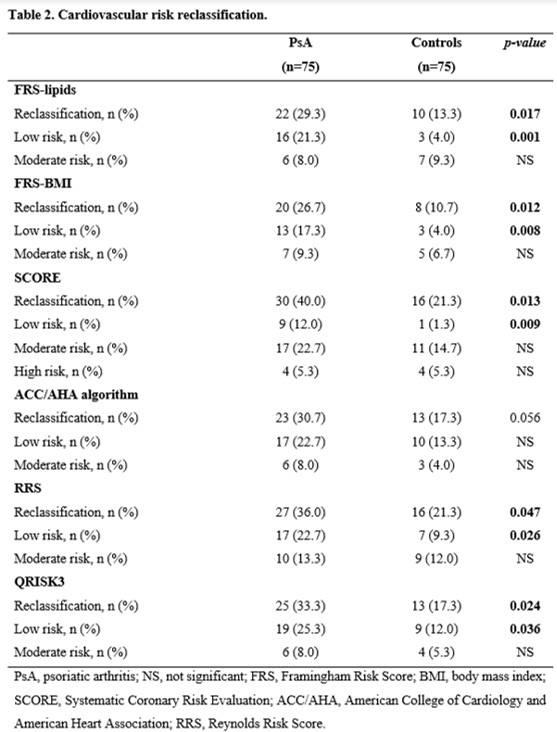
Results: Mean age was 53.89 ± 10.59 in PsA patients and 54.25 ± 7.08 in the control group (p=0.807), 57.3% were women in both groups. There were no significant differences in traditional CVR factors between PsA patients and controls. A difference was found in the presence of CP, being more prevalent in PsA patients (44.0% vs 26.7%, p=0.026) and in the presence of subclinical atherosclerosis overall (52.0% vs 34.7%, p=0.032) (Table 1). When comparing the CVR reclassification to a higher risk category a difference was found in five of the six CVR algorithms. The reclassification was more prevalent in PsA patients: 29.3% vs 13.3%, p=0.017 with FRS-lipids; 26.7% vs 10.7%, p=0.012 with FRS-BMI; 40.0% vs 21.3%, p=0.013 with SCORE; 33.3% vs 17.3%, p=0.024 with QRISK3; and 36.0% vs 21.3%, p=0.047 with RRS (Table 2).
Conclusion: The CVR algorithms underestimate de real CVR of PsA patients. This could be attributed to the fact that these algorithms do not include disease characteristics that can affect the CV prognosis of PsA patients. For this reason, a carotid US should be done to correctly classify the CVR of PsA patients and identify those who would benefit from an opportune treatment.
To cite this abstract in AMA style:
Guajardo-Jauregui N, Colunga-Pedraza I, Azpiri-Lopez J, Galarza-Delgado D, Rodriguez-Romero A, Flores-Alvarado D, Meza-Garza A, Loya-Acosta J, Cardenas-de La Garza J, Lugo-Perez S, Ilizaliturri-Guerra O, Garcia-Arellano G, Castillo-Treviño J. Cardiovascular Risk Reclassification According to Six Traditional Cardiovascular Risk Algorithms and a Carotid Ultrasound in Psoriatic Arthritis Patients [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/cardiovascular-risk-reclassification-according-to-six-traditional-cardiovascular-risk-algorithms-and-a-carotid-ultrasound-in-psoriatic-arthritis-patients/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-risk-reclassification-according-to-six-traditional-cardiovascular-risk-algorithms-and-a-carotid-ultrasound-in-psoriatic-arthritis-patients/