Session Information
Date: Sunday, November 8, 2015
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose : Our aim was 1) to analyze the association between demographic and traditional cardiovascular risk factors (CVRF) and cardiovascular disease (CVD) in subjects affected with rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), psoriasis (Ps), psoriatic arthritis (PsA), Crohn’s disease (CD), or ulcerative colitis (UC), and 2) to compare the standardized prevalence of CVD among these conditions.
Methods : Subjects included in this cross-sectional study were collected as part of the Immune-Mediated Inflammatory Disease Consortium between 2007-2010. Demographic and clinical data was collected using standardized questionnaires during a clinical interview with close questions and review of medical records. Multivariate logistic regression models adjusted by demographic (gender, age, educational level, elapsed time from IMID diagnosis) and traditional CVRF [dyslidepemia (DL), type 2 diabetes (T2D), obesity (OB), ever smoking] were constructed for each IMID. Results for each variable were combined using inverse variance weighted metaanalysis. Standardized prevalence for each IMID, adjusted by demographic and traditional CVRF [per 100 patients, with 95% confidence intervals (CI)] was calculated using marginal analysis.
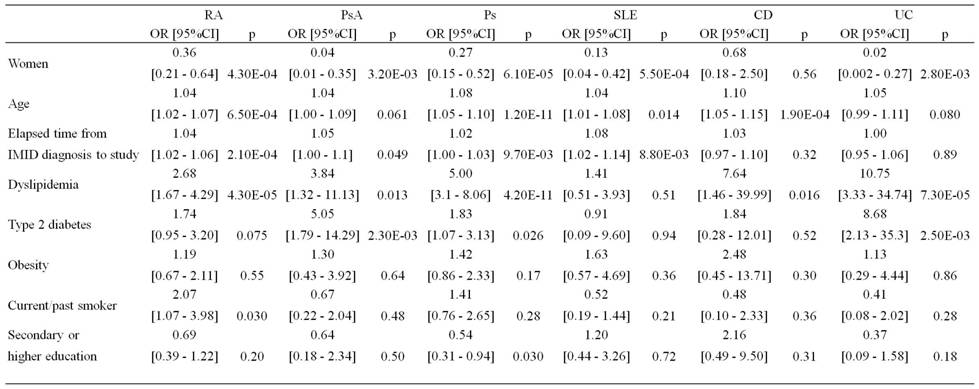
Results: 9951 patients were included (Table 1). Table 2 shows the association between demographic and traditional CVRF and CVD in each IMID. When results from the 6 cohorts were combined, males, lower educational level, older age and more time elapsed from disease diagnosis, and presence of DL and T2D were independently associated with a higher risk of CVD. SLE exhibited the highest standardized prevalence, followed by RA, Ps, CD, PsA and UC (Figure 1).
Conclusion : The contribution to CV risk of demographic and traditional CVRF is different for each IMID. SLE showed the higher standardize prevalence of CVD when compared to other IMIDs.
Table 1: Demographic characteristics and prevalence of CVD disease and traditional CV risk factors of the patients included in this study.
|
|
RA (n = 2152) |
PsA (n = 1147) |
Ps (n = 2497) |
SLE (n = 760) |
CD (n = 1938) |
UC (n = 1457) |
|
Age, (n) X (IQR) |
(1996) 61 (52 to 70) |
(1113) 52 (41.09 to 63) |
(2430) 47 (36 to 59) |
(702) 44 (35 to 55) |
(1913) 39 (32 to 49) |
(1436) 47 (37 to 58.12) |
|
Women, n (%) |
1.567 (77.69) |
522 (47.28) |
1.057 (43.46) |
671 (93.19) |
956 (49.84) |
663 (46.01) |
|
Calendar year at IMID diagnosis, (n) X (IQR) |
(2144) 1998 (1991 to 2004) |
(1137) 2003 (1996 to 2007) |
(2482) 1992 (1980 to 2001) |
(678) 1999 (1993 to 2004) |
(1314) 1998 (1993 to 2002) |
(975) 1998 (1993 to 2002) |
|
Elapsed time from IMID diagnosis to study§, in years , (n) X (IQR) |
(2132) 10 (5 to 17) |
(1076) 7 (3 to 13) |
(2480) 17 (8 to 29) |
(675) 10 (6 to 17) |
(1313) 10 (6 to 15) |
(975) 10 (7 to 16) |
|
Secondary or higher education, n (%) |
655 (33.73) |
449 (44.46) |
1278 (54.20) |
378 (54.00) |
1187 (62.77) |
785 (55.48) |
|
CVD, n (%) |
91 (4.23) |
24 (2.09) |
94 (3.76) |
24 (3.16) |
14 (0.72) |
22 (1.51) |
|
Current/past smoker, n (%) |
828 (49.49) |
533 (59.55) |
1.411 (69.68) |
369 (62.02) |
1.282 (74.62) |
727 (62.08) |
|
Arterial hypertension, n (%) |
638 (29.65) |
– |
476 (19.06) |
178 (23.42) |
123 (6.35) |
148 (10.16) |
|
Dyslipidemia, n (%) |
433 (20.12) |
157 (13.69) |
436 (17.46) |
125 (16.45) |
68 (3.51) |
127 (8.72) |
|
Type 2 diabetes, n (%) |
172 (7.99) |
92 (8.02) |
203 (8.13) |
24 (3.16) |
28 (1.44) |
55 (3.77) |
|
Obesity, n (%) |
366 (19.02) |
250 (24.56) |
612 (25.82) |
102 (15.36) |
184 (9.97) |
198 (14.25) |
|
Number of DMARDs, X [IQR] |
2 (1-3) |
1 (0-2) |
0 (0-0) |
2 (1-2) |
1 (0-1) |
0 (0-1) |
|
Patients with biological drugs, n (%) |
914 (42.47) |
299 (26.07) |
493 (19.74) |
47 (6.18) |
282 (14.55) |
70 (4.80) |
Table 2: Multivariate logistic regression models to analyze the influence of demographic and traditional cardiovascular (CV) risk factors in the prevalence of CV disease in each of our 6 cohorts.
Figure 1: Standardized prevalence of cardiovascular disease, with 95% confidence intervals, for each IMID.
To cite this abstract in AMA style:
Rodriguez-Rodriguez L, Perrotti PP, Aterido A, Tornero J, Ferrandiz C, Cañete JD, Fernandez-Nebro A, Gisbert JP, Domènech E, López-Lasanta M, Marsal S, Fernández-Gutiérrez B. Cardiovascular Disease in Immune-Mediated Inflammatory Diseases: Cross Sectional Analysis of the Influence of Demographic and Traditional Cardiovascular Risk Factors [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/cardiovascular-disease-in-immune-mediated-inflammatory-diseases-cross-sectional-analysis-of-the-influence-of-demographic-and-traditional-cardiovascular-risk-factors/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-disease-in-immune-mediated-inflammatory-diseases-cross-sectional-analysis-of-the-influence-of-demographic-and-traditional-cardiovascular-risk-factors/