Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Extensive skin disease and renal crisis are hallmarks of anti-RNA polymerase III (RNAP) positive systemic sclerosis (SSc), while data on lung and heart involvement are conflicting. Here, the aims were to perform time-course analyses of interstitial lung disease (ILD) and pulmonary hypertension (PH) in the RNAP subset in a prospective unselected SSc cohort with longitudinal follow up data and use the other auto-antibody subsets as comparators. <>Methods:
The study cohort included 276 SSc patients from the observational Oslo University Hospital cohort with complete data on (A) SSc-related auto-antibodies, (B) paired, serial analyses of lung function and extent of fibrosis by lung HRCT at baseline and follow-up, and (C) PH verified by right heart catheterization. All patients in the SSc cohort met the 2013 ACR/EULAR classification criteria.Results:
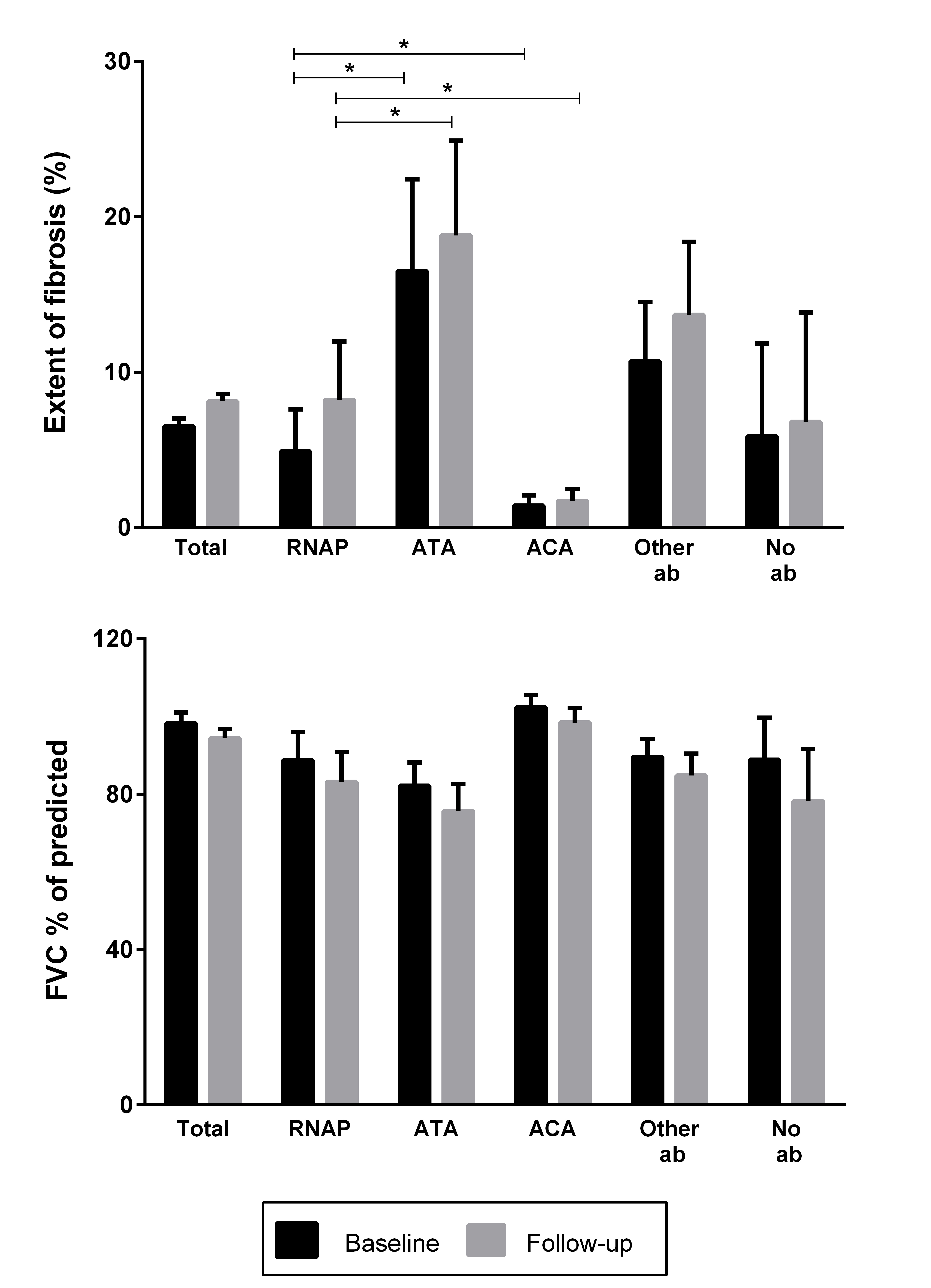
RNAP was positive in 33/276 patients (12%), of which 79% had diffuse cutaneous SSc. Patients with RNAP had higher modified Rodnan Skin Score, developed more frequently scleroderma renal crisis and gastric antral vascular ectasia than anti-Topoisomerase 1 (ATA) and anti-centromere antibody (ACA) positive patients. Pulmonary findings in the RNAP subset were heterogeneous; 49% had no signs of ILD, while 33.3% had moderate fibrosis (1-20% fibrosis) and 18.2% had severe fibrosis at follow up (>20% fibrosis); (Figure 1 and 2). The annual fibrosis progression rate was higher in RNAP (1.2% SD 2.0) compared to ATA (0.5%, SD 5.0) and ACA (0.7%, SD 1.4) but did not reach statistical significance. Forced Vital Capacity at follow up was <80% in 39% of the RNAP subset; comparable to the anti-topoisomerase subset (ATA: 47%), but higher than anti-centromere (ACA: 13%). The accumulated frequency of PH in the RNAP subset (12 %) was lower than in ACA (18 %). The 5- and 10 year survival rates in RNAP cases were 93% and 78%, respectively. The survival of RNAP positive patients was comparable to the ATA and ACA subsets, but significantly higher than in the ANA negative patient subset.Conclusion:
In this cohort, the RNAP subset was marked by cardiopulmonary heterogeneity with progression to extensive ILD in 18 %, and PH development in 12 %. These data indicate that cardiopulmonary risk stratification early in the disease course is particularly important in RNAP positive SSc.
Disclosure: A. Hoffmann-Vold, None; A. Heiervang Tennøe, None; O. Midtvedt, None; M. B. Lund, None; T. Garen, None; F. El-Hage, None; T. M. Aalokken, None; E. Taraldsrud, None; Ø. Molberg, None.
To cite this abstract in AMA style:
Hoffmann-Vold A, Heiervang Tennøe A, Midtvedt O, Lund MB, Garen T, El-Hage F, Aalokken TM, Taraldsrud E, Molberg Ø. Cardiopulmonary Disease Development in Anti-RNA Polymerase III Positive Systemic Sclerosis; Comparative Analyses from an Unselected, Prospective Patient Cohort [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/cardiopulmonary-disease-development-in-anti-rna-polymerase-iii-positive-systemic-sclerosis-comparative-analyses-from-an-unselected-prospective-patient-cohort/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiopulmonary-disease-development-in-anti-rna-polymerase-iii-positive-systemic-sclerosis-comparative-analyses-from-an-unselected-prospective-patient-cohort/