Session Information
Date: Tuesday, October 28, 2025
Title: (2015–2051) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Ankylosing Spondylitis (AS) is a subtype of spondyloarthritis (SpA), a group of inflammatory diseases. AS is influenced by a complex interplay of factors arising from both autoimmune and autoinflammatory mechanisms, with key contributors including HLA-B27, alterations in the IL-23 signaling pathway, and mutations in the MEFV gene. Among these factors, MEFV gene mutations are the cause of familial Mediterranean fever (FMF), which is considered one of the prototypes of autoinflammatory diseases. In the treatment of FMF, the primary targeted pathways are microtubules and IL-1 pathways, which aim to reduce inflammation through autoinflammatory mechanisms. In this study, we aimed to investigate whether treating FMF with drugs that inhibit autoinflammatory pathways could also lead to a reduction in the symptoms of AS in patients diagnosed with both FMF and AS.
Methods: In this study, 28 patients were enrolled, all of whom had been diagnosed with both Ankylosing Spondylitis (AS) and Familial Mediterranean Fever (FMF) based on the 1984 Modified New York Criteria and Tel-Hashomer Criteria, respectively. Each patient was contacted and asked about the severity of their AS using the BASDAI and VAS back pain scores before and after colchicine treatment, as well as other IL-1 treatments. Additional information, such as M694V mutations, was obtained from their hospital records.
Results: Twenty-eight patients were included in our study. The mean age of the patients was 44.89 ± 10,9 years. The mean duration of AS and FMF was 12.35±6,95 years and 17.71±7,72 years, respectively. The impact of colchicine on AS severity was assessed using the BASDAI score before and after treatment. The results were not significant for the BASDAI score (p =0,068). Patients were evaluated using the VAS back pain score before and after colchicine treatment. The results were similarly non-significant (p=0,145)(Table 2). The BASDAI score improvements before and after treatment for patients using canakinumab and anakinra showed no significant results (p > 0.05). Among the 28 patients, 6 had the M694V homozygous mutation, and 9 had the M694V heterozygous mutation. BASDAI scores before and after colchicine treatment showed a significant difference in M694V homozygous patients (p=0,048). No such improvement in BASDAI scores was observed in patients with M694V heterozygous mutations (p=0,47). VAS back pain scores before and after treatment in M694V homozygous patients also showed significant improvement after colchicine treatment (p=0,011). Similarly to the BASDAI scores, VAS back pain scores remained non-significant in M694V heterozygous patients before and after treatment (p =0,217).
Conclusion: Although colchicine and other IL-1 targeted therapies did not lead to significant clinical improvement in the overall ankylosing spondylitis (AS) patient population, a notable exception was observed in individuals homozygous for the M694V mutation. In this subgroup, colchicine treatment was associated with marked reductions in both BASDAI and VAS back pain scores, suggesting a potential genotype-specific therapeutic response that warrants further investigation.
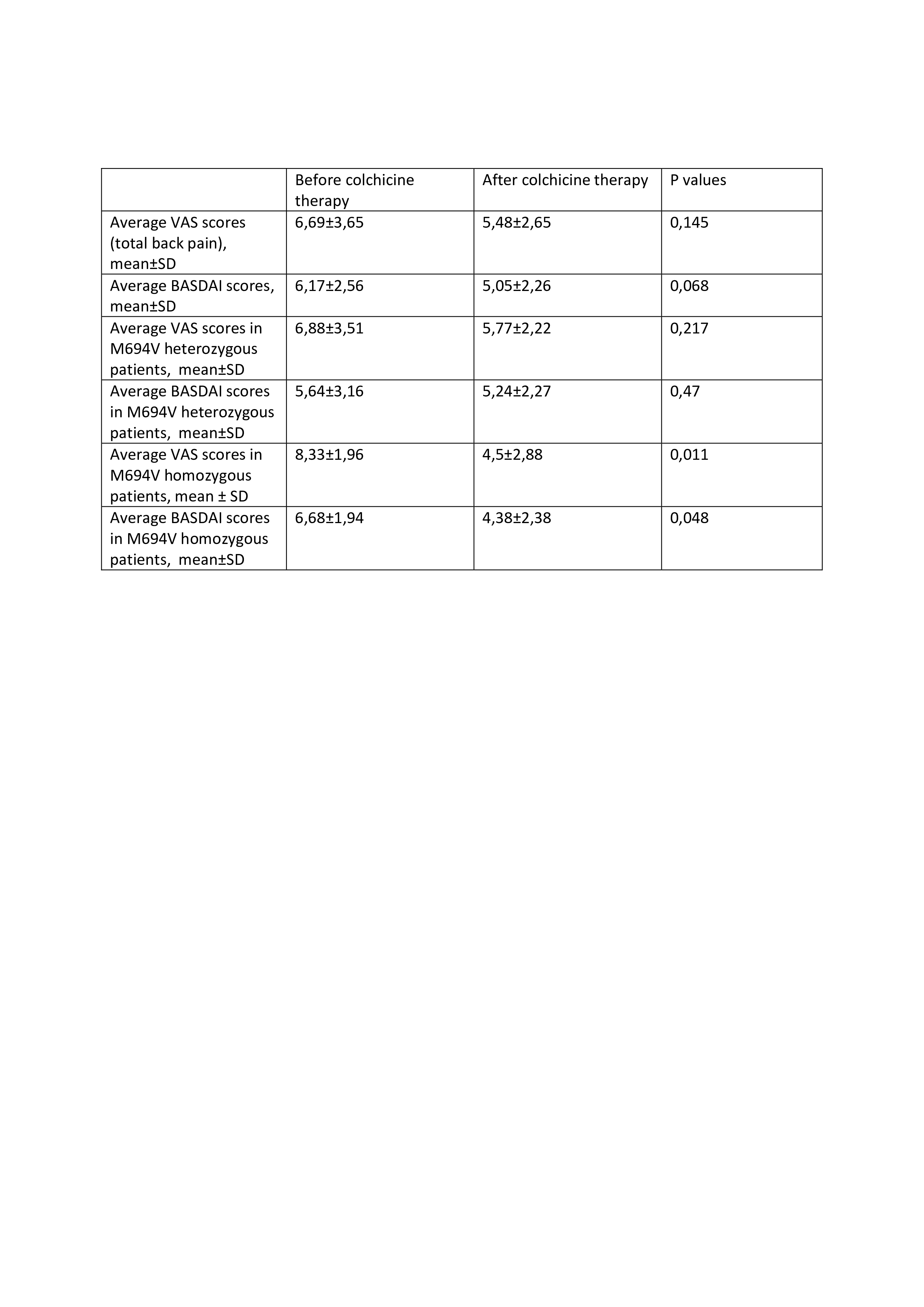 Table 1- Patient’s clinical scores before and after the treatment
Table 1- Patient’s clinical scores before and after the treatment
To cite this abstract in AMA style:
Ates M, Ugurlu s. Can Colchicine Be a Therapeutic Option for Patients with Ankylosing Spondylitis? [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/can-colchicine-be-a-therapeutic-option-for-patients-with-ankylosing-spondylitis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/can-colchicine-be-a-therapeutic-option-for-patients-with-ankylosing-spondylitis/
