Session Information
Date: Monday, November 6, 2017
Title: Spondyloarthropathies and Psoriatic Arthritis – Pathogenesis, Etiology
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Studies that compare the immune cell phenotype or function from patients with psoriatic arthritis (PsA) to patients with psoriasis limited to cutaneous involvement (Pso) are exceedingly scarce, particularly in patients without immune-modulatory medications that confound results. A head-to-head comparison of the immune cell composition in PsA and Pso is an essential step to understand the development of rheumatic manifestations in patients with psoriasis.
Methods: Blood samples and clinical parameters were collected from 23 healthy controls (HC), 21 patients with psoriasis in whom psoriatic arthritis was excluded by a rheumatologist (Pso), 21 patients with psoriatic arthritis meeting CASPAR criteria (PsA) and 16 patients with ankylosing spondylitis meeting ASAS criteria but without psoriasis (AS). The Pso and PsA cohorts were matched for age, gender, CRP, ESR, psoriasis duration and psoriasis skin severity. All patients were free from biological or conventional DMARD therapy. Using a highly standardized flow-cytometric protocol the peripheral blood mononuclear cells (PBMCs) from patients and controls underwent extensive extracellular and intracellular immunophenotyping capable of detecting over 110 different myeloid and lymphoid cell subsets / populations. In synovial fluid (SF) samples from patients with psoriatic arthritis the level of CCL27 was determined using Luminex Technology and the presence of CCR10+ CD8 T cells was evaluated by flow-cytometry.
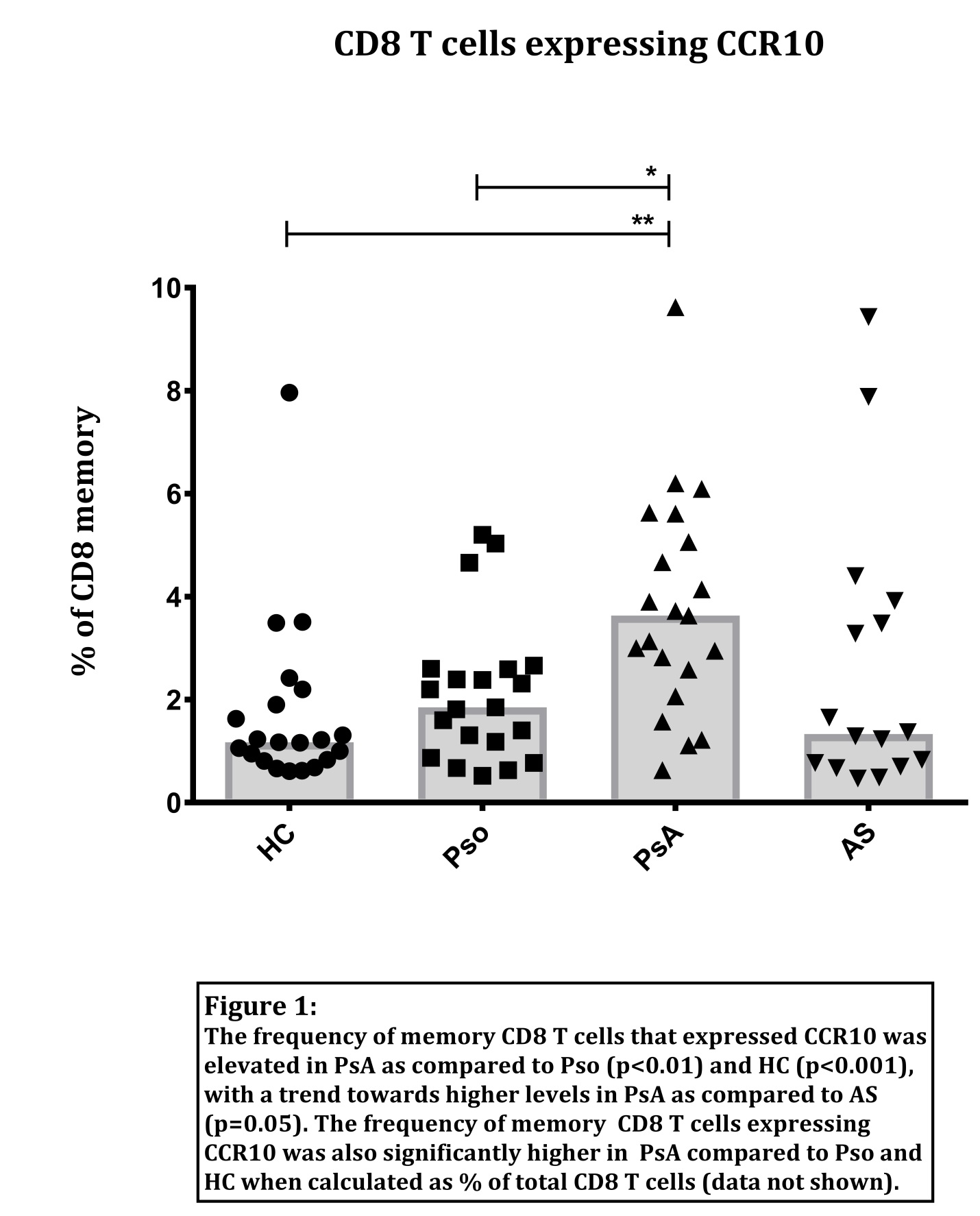
Results: The overall phenotype and immune cell composition showed remarkable overlap in PsA and Pso, with both cohorts characterized by an increase in the frequency of regulatory T cells, an increase in IL-17A & IL-22 co-producing CD4 and CD8 T cells, a decrease in plasmacytoid dendritic cells, and a decrease in mucosal-associated invariant T (MAIT)-like cells. Only one specific cell population differentiated the PsA from Pso cohort: CCR10+ CD8 T cells, being enriched in PsA as compared to Pso (Figure 1). These CCR10+ CD8 T cells had an effector memory status, were CXCR3-CCR6- and predominantly co-expressed CCR4. While the CCR4+ CD8 T cell frequencies were positively correlated to psoriasis skin severity, the CCR10+ CD8 T cell frequencies were not related to skin severity. Analysis of SF samples from psoriatic arthritis patients confirmed the presence of CCL27, the ligand for CCR10 receptor, and the expression of CCR10 on SF CD8 T cells.
Conclusion: A broad immunophenotyping strategy has revealed a potentially novel role for CD8 T cells expressing CCR10 to mediate the progression from cutaneous disease to joint disease in psoriatic arthritis. Further functional studies are needed to investigate the role these cells play in the different compartments affected by the disease.
To cite this abstract in AMA style:
Leijten EFA, van Kempen TS, Olde Nordkamp MAM, Verhagen FH, Hiddingh S, Kuiper JJW, Boes ML, Radstake TRDJ. Broad Immunophenotyping Results: CCR10 Expressing CD8 T Cells Distinguish Psoriatic Arthritis from Psoriasis Limited to Skin Involvement [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/broad-immunophenotyping-results-ccr10-expressing-cd8-t-cells-distinguish-psoriatic-arthritis-from-psoriasis-limited-to-skin-involvement/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/broad-immunophenotyping-results-ccr10-expressing-cd8-t-cells-distinguish-psoriatic-arthritis-from-psoriasis-limited-to-skin-involvement/