Session Information
Date: Tuesday, October 28, 2025
Title: (2227–2264) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis (RA) is a well-established risk factor for fractures, due to both systemic inflammation and treatment-related effects on bone metabolism. This study aimed to identify clinical factors contributing to BMD decline and fracture under current RA and osteoporosis treatment strategies.
Methods: We conducted a retrospective cohort study at a university hospital in Japan, including RA patients with at least two dual-energy X-ray absorptiometry (DXA) scans of the femoral neck between 2010 and 2024. Group-based trajectory modeling (GBTM) was used to classify patients according to longitudinal BMD changes over 7 years since the initial measurement. Baseline characteristics and treatment exposures during follow-up were compared across the identified trajectory groups. Factors associated with BMD trajectory were explored using multinomial logistic regression. Incident fractures during the observation period were also assessed for each group.
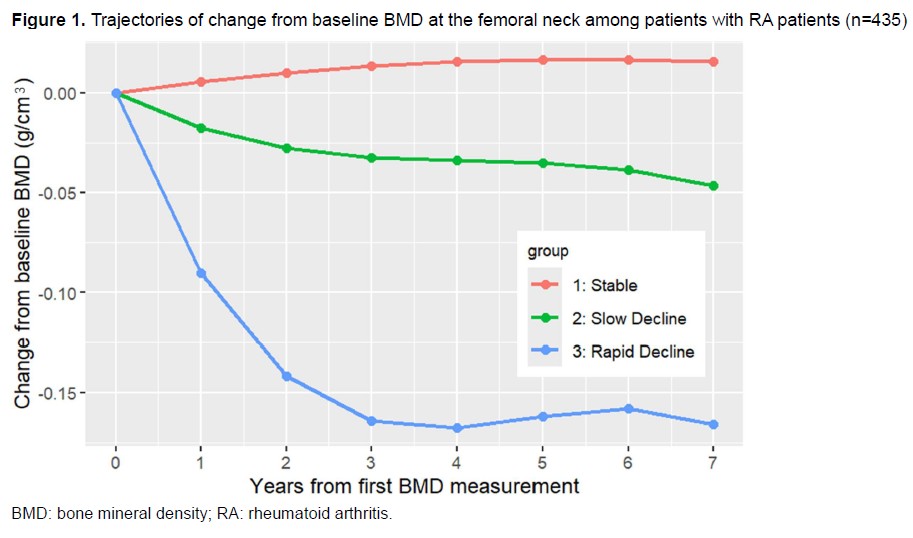
Results: We analyzed 1,681 BMD measurements from 435 RA patients (mean age: 62 years; 78% female; 81% seropositive). GBTM identified three distinct BMD trajectory groups: Stable (n=211), Slow Decline (n=149), and Rapid Decline (n=75) (Figure 1). The Stable group had the lowest baseline BMD (mean: 0.59 g/cm³), while the Rapid Decline group had the highest (mean: 0.76 g/cm³). Use of denosumab and vitamin D supplements was significantly higher in the Stable group, whereas glucocorticoid use was more prevalent in the Rapid Decline group (Table 1). Multivariable analysis revealed that older age, female sex, and higher baseline BMD were independently associated with the Rapid Decline trajectory (ORs: age 1.05 [95%CI 1.02 to 1.09], female 2.79 [95%CI 1.10 to 7.05], BMD 3.92 [2.76 to 5.58]). Additionally, the use of osteoporosis medications was negatively associated with decline trajectories (Table 2). The incidence of new fractures per 100 person-years was 1.49 in the Stable group, 2.79 in the Slow Decline group, and 2.06 in the Rapid Decline group, with no statistically significant difference (p=0.20).
Conclusion: This 7-year longitudinal analysis identified three distinct BMD trajectories in RA patients. Notably, those in the Rapid Decline group had relatively high baseline BMD but did not exhibit lower fracture rates. The higher prevalence of glucocorticoid use and lower use of osteoporosis treatment in the decline groups suggest that suboptimal osteoporosis management may contribute to accelerated BMD loss and fracture risk, even in patients with initially preserved bone density. These findings highlight the need for proactive osteoporosis prevention strategies throughout the course of RA.
To cite this abstract in AMA style:
Hirose K, Hayashi K, Kubota N, Terajima Y, Matsumoto K, Nakadoi T, Nawachi S, Miyawaki Y, Katsuyama E, Katsuyama T, Watanabe H, Narazaki M, Matsumoto Y, Wada J. Bone Mineral Density Trajectories and Fracture Risk in Rheumatoid Arthritis: A 7-Year Longitudinal Analysis Using Group-Based Trajectory Modeling [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/bone-mineral-density-trajectories-and-fracture-risk-in-rheumatoid-arthritis-a-7-year-longitudinal-analysis-using-group-based-trajectory-modeling/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-mineral-density-trajectories-and-fracture-risk-in-rheumatoid-arthritis-a-7-year-longitudinal-analysis-using-group-based-trajectory-modeling/

.jpg)
.jpg)