Session Information
Date: Tuesday, November 12, 2019
Title: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: To evaluate alterations of bone mineral density and microarchitecture in patients with rheumatoid arthritis (RA). We also aimed to identify potential factors associated with these alterations.
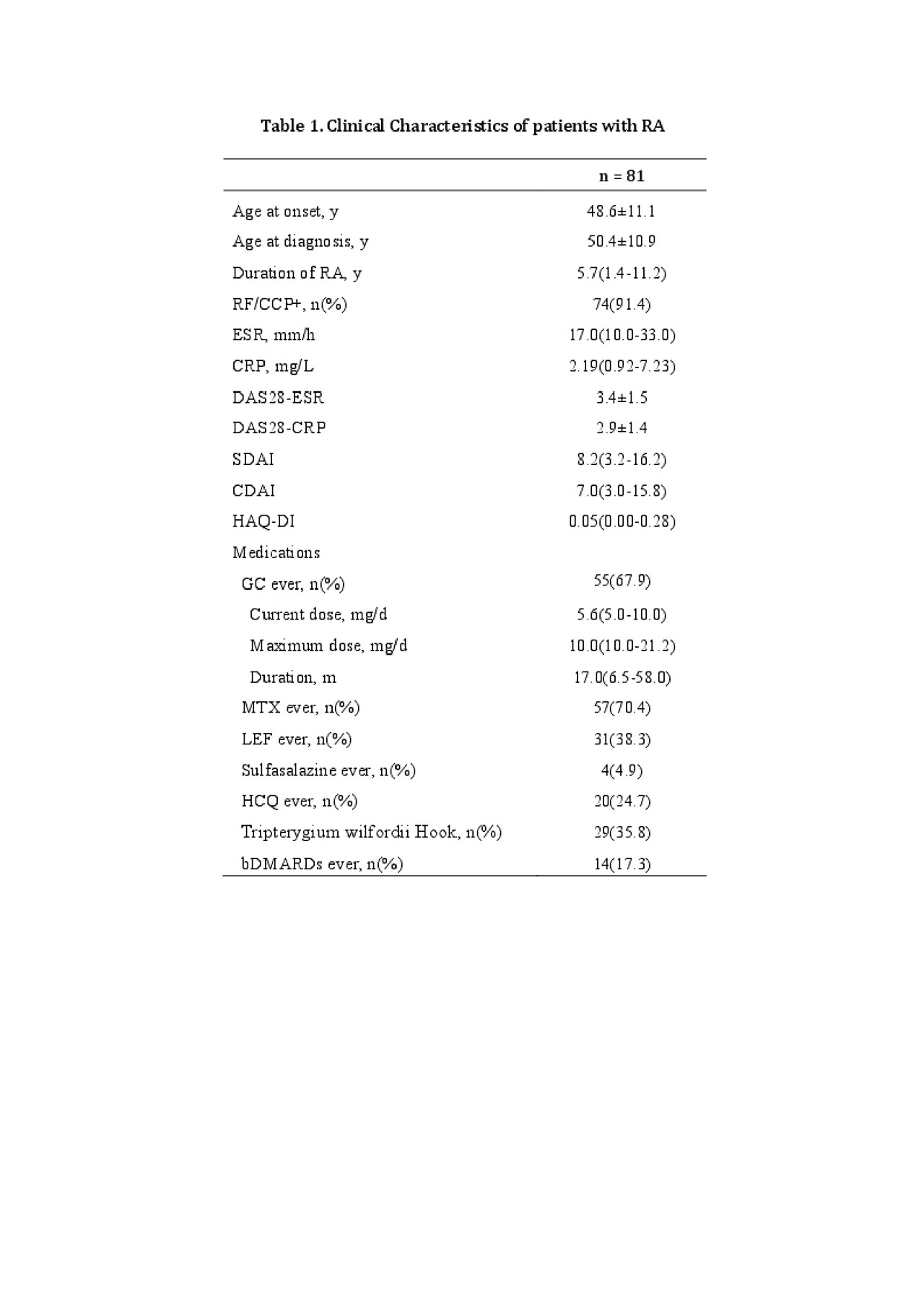
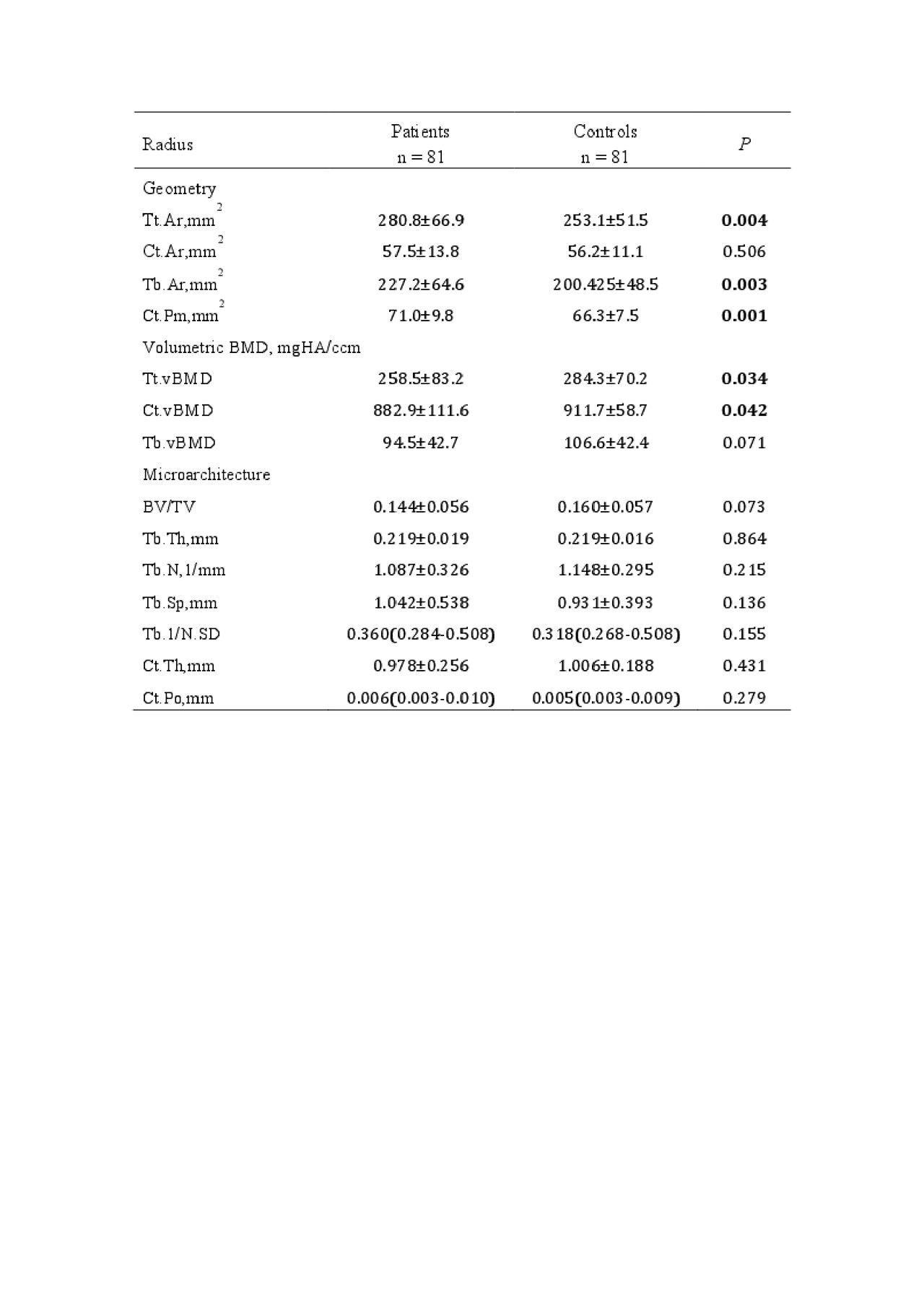
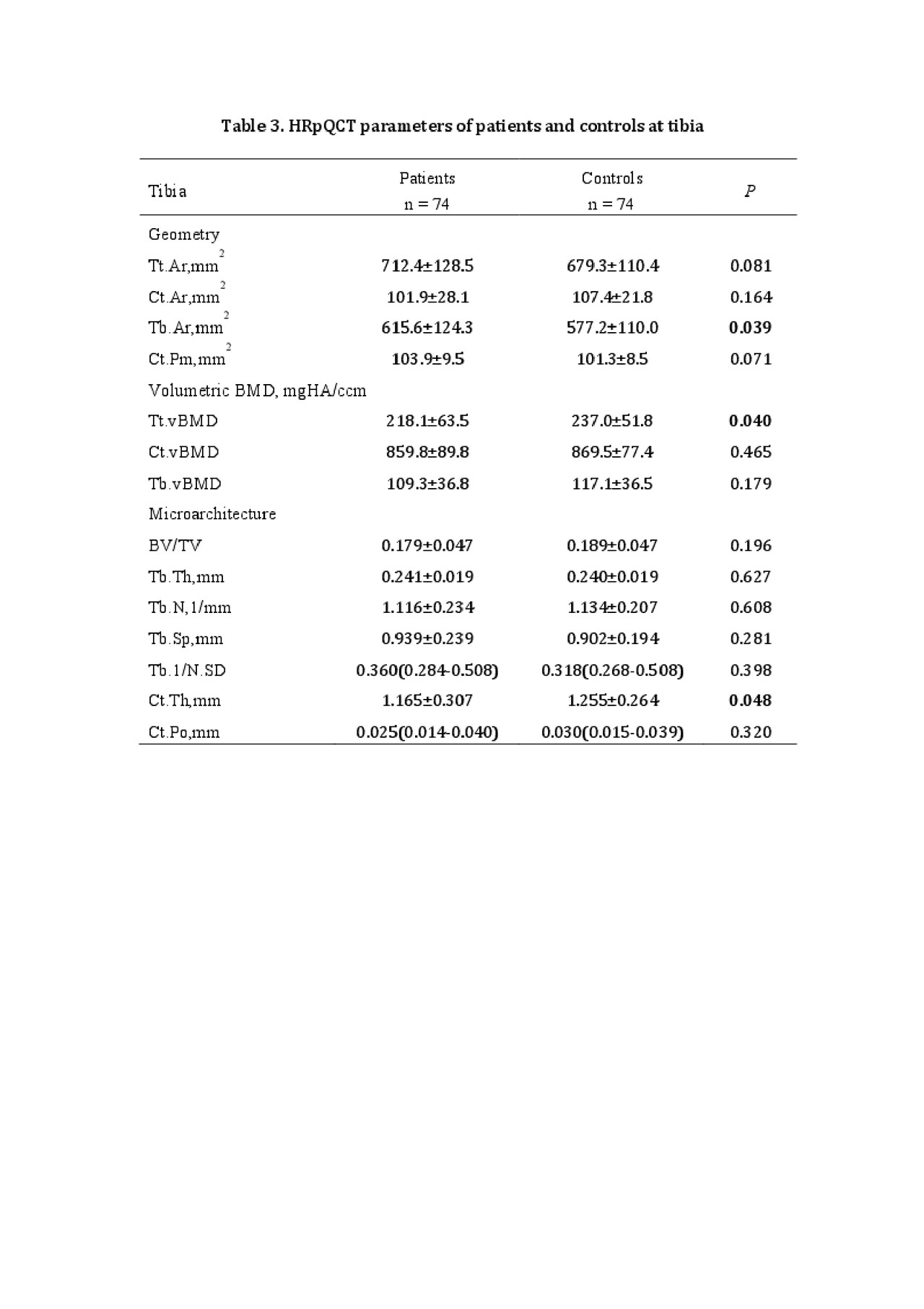
Methods: In this case-control study, patients with RA were recruited from the PUMC Hospital site of the Chinese Registry of rhEumatoiD arthrITis (CREDIT). The primary outcomes were high-resolution peripheral quanitative computed tomography (HRpQCT)-related measures at the distal radius and tibia (Scanco XtremeCT II), and data from age- and gender-matched healthy controls were included for comparison. Additional diagnostic imaging examinations included thoracolumbar X-ray and DXA. Data regarding demographic and clinical characteristics, osteoporosis-related risk factors, and RA-related diagnosis and treatment history were collected. Finally, grip srength, serum bone turnover markers, TNF-α and IL-6 were also measured. Correlation between HRpQCT parameters and potentially related covariates were analyzed using univariate and multivariate linear regression analysis.
Results: A total of 81 patients (69 women, aged 57.9±8.7y, RA duration 5.7(1.4-11.2)y) and 81 matched healthy controls were included. Compared with controls, patients had significantly larger bone area and lower total and trabecular vBMD at both distal radius and tibia. HRpQCT measures at the distal tibia also showed lower cortical bone thickness in patients with RA. Further analyses were conducted among RA patients. aBMD at both the lumbar spine and total hip was positively correlated with vBMD, trabecular bone volume fraction, trabecular number and cortical thickness, and was negatively correlated with trabecular separation and inhomogeneity. Trabecular thickness and cortical porosity were not correlated with aBMD at any sites. vBMD was positively correlated with body mass index, grip strength and ever being treated with HCQ, and was negatively associated with age, RA duration and DAS28-ESR. Age and RA duration were significant factors in multivariate analysis. In contrast, parameters reflecting impairment of microarchitecture (trabecular inhomogeneity and separation) were negatively correlated with BMI and grip strength, and was positively related to age, disease duration and activity. Duration and activity remained significant in multivariate regression. Current treatment with glucocorticoids was related to decreased vBMD, trabecular number and increased trabecular separation and inhomogeneity. No correlations were observed with regards to dose or duration of GCs. Patients with fragility fractures had significantly lower vBMD in both trabecular and cortical bone, thinner cortical bone as well as impaired trabecular bone microstructure (fewer in number, larger separation and increased inhomogeneity). Bone turnover markers, TNF-α and IL-6 were not related to any HRpQCT parameters in this study.
Conclusion: Patients with RA have alterations in bone density and microarchitecture compared to healthy population, which may impair bone strength and lead to increased risk of fractures. Both traditional risk factors for osteoporosis and RA-associated factors need to be considered in the assessment of bone quality in RA.
To cite this abstract in AMA style:
Jin S, Hsieh E, Xia W, Li M, Wang Q, Zeng X. Bone Mineral Density and Microarchitecture Among Chinese Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/bone-mineral-density-and-microarchitecture-among-chinese-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-mineral-density-and-microarchitecture-among-chinese-patients-with-rheumatoid-arthritis/