Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Major adverse cardiovascular events (MACE) are known comorbidities and consequences of psoriasis (PsO) and psoriasis arthritis (PsA). Previous studies underlined the potential of immunomodulatory agents decreasing MACE incidence in patients with PsO and PsA.
We aimed to assess the risk of developing MACE in patients with pre-existing PsO treated with different treatment regimens; topical treatment, methotrexate and biologic disease-modifying anti-rheumatic drugs (bDMARDs), including antiTNFα, anti-IL17 and anti-IL12/23 agents and JAK inhibitors.
Methods: We conducted a retrospective exploratory study using real-world data from the databases of ‘Meuhedet’, the third-largest Israeli health maintenance organization, covering approximately 1.3 million subjects. A total of 55,780PsO and 5,223 PsA patients were diagnosed between January 2000 and January 2020 and 244,012 healthy controls were included. We performed Cox proportional hazards regression analysis adjusted for factors including sex, body mass index, age at PsO diagnosis, diagnosis of type 2 diabetes mellitus, dyslipidemia, and hypertension. To gain further insight into the influence of different types of bDMARDs on the risk of MACE, we undertook a comprehensive logistic regression analysis which included the accumulative constatives of the different types of bDMARDs and the mean quantity per month with the same adjustments as in the cox analysis.
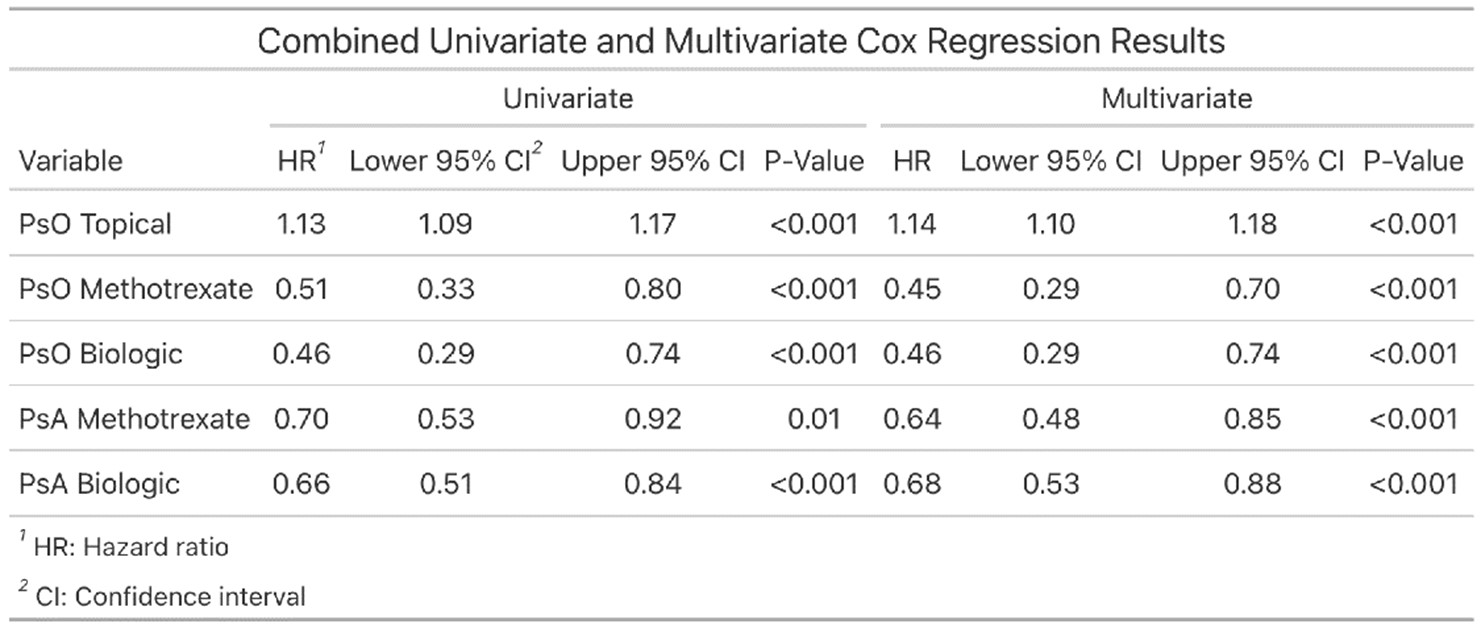
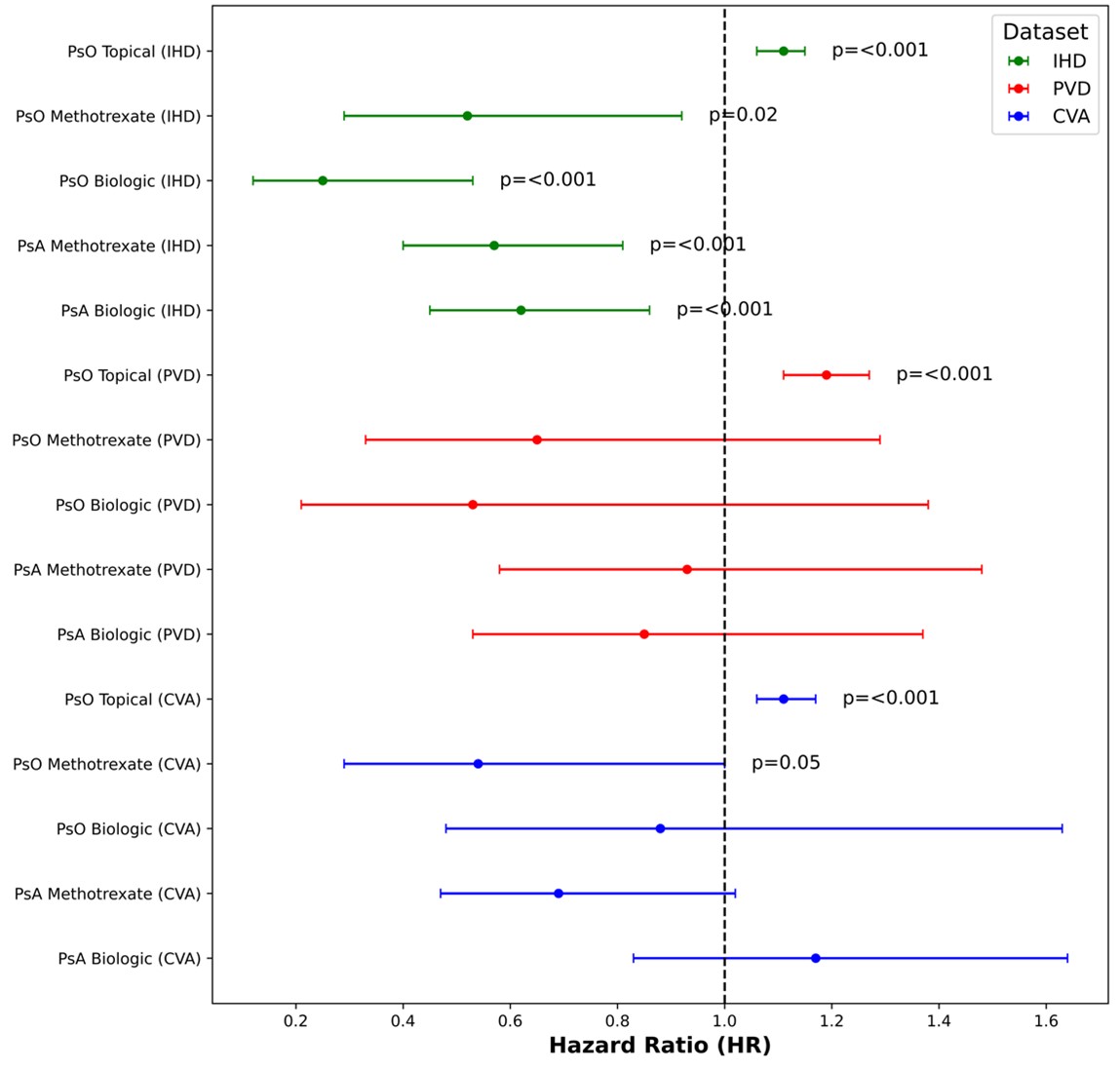
Results: After implementing the exclusion criteria, our study comprised 216,896 participants, with 52,632PsO and 1,592 PsA patients and 162,672 matched controls, contributing a total of 2,261,815 patient-years. PsO and PsA patients treated with methotrexate or bDMARDs showed a significantly lower MACE risk compared to health matched controls (HR: 0.45-0.68, p-value: < 0.001). However, patients receiving topical therapy exhibited a marginally increased MACE risk compared to health matched controls (HR: 1.14, p-value: < 0.001) (Table 1). Individual outcomes constituting the composite of MACE, including cerebrovascular accidents, ischemic heart disease, and peripheral vascular disease, showed similar trends(Figure 1).In the logistic regression analysis of PsO and PsA patients exclusively treated with biological treatments, we observed stronger cardioprotective properties of anti-IL-12/23 and anti-IL-17 compared to anti-TNF. Importantly, increased mean monthly quantity of anti-TNF was associated with higher risk of developing MACE (OR=1.12, p=0.042, 95% CI [1.01, 1.24]).In contrast, total quantity of anti-IL 17, anti-IL 12/23, and JAKi reduced risk of developing MACE (OR = 0.98, p = 0.024, CI [0.96, 0.99]).
Conclusion: Our findings suggest that systemic anti-inflammatory treatments for PsO and PsA, including bDMARDs and methotrexate, provide cardioprotective effects. Our study also highlights potential cardiovascular benefits of anti-IL17 and anti-IL12/23 biological agents compared to anti-TNF treatments. This information can assist clinicians and patients in making informed decisions about these therapeutic agents.
To cite this abstract in AMA style:
Dotan A, Ben-Shabbat N, watad A, McGonagle D, AMITAL H. Biological Therapies for Psoriasis and Psoriatic Arthritis- effects on Future Risk Development of Major Adverse Cardiovascular Events (MACE) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/biological-therapies-for-psoriasis-and-psoriatic-arthritis-effects-on-future-risk-development-of-major-adverse-cardiovascular-events-mace/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/biological-therapies-for-psoriasis-and-psoriatic-arthritis-effects-on-future-risk-development-of-major-adverse-cardiovascular-events-mace/