Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a heterogeneous autoimmune rheumatic disease whose prognosis varies by race and sex. To understand whether the cognitive processes of clinical decision-making influence the diagnosis of SLE, we conducted a factorial survey experiment to evaluate variation in primary care providers’ (PCP) diagnosis of SLE when all aspects of a clinical case are held constant, with the exception of race and sex.
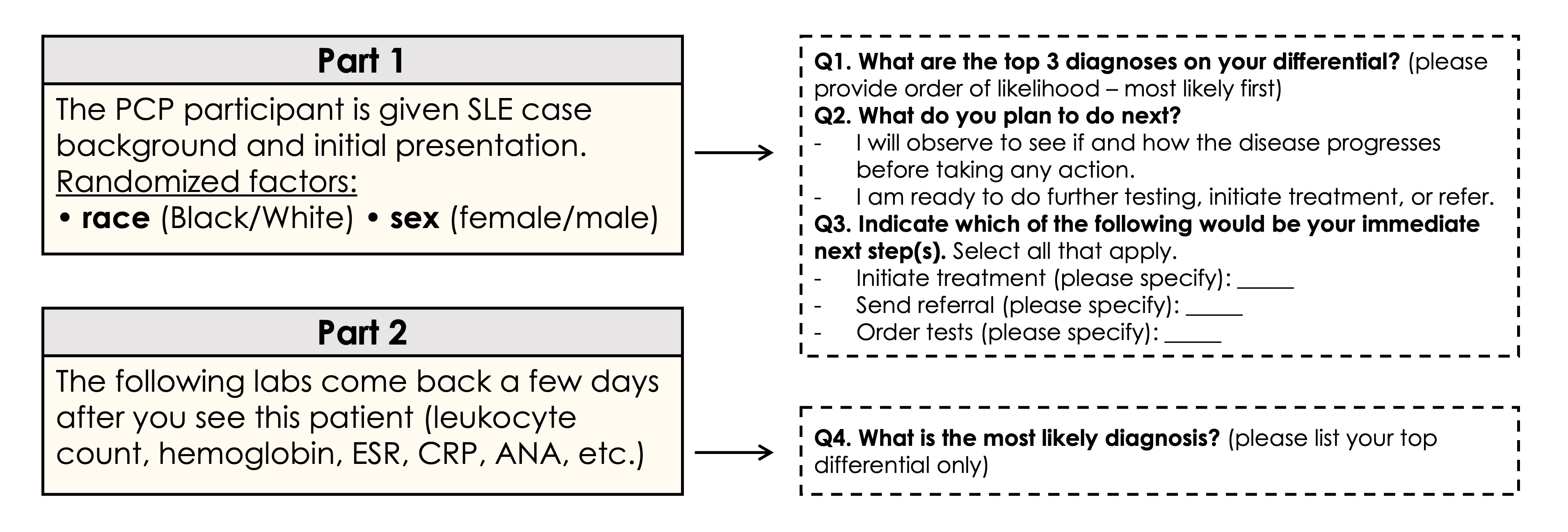
Methods: An online survey was distributed via email from 04/11/2024 to 06/10/2024 to PCPs across the US. Participants were presented with five clinical vignettes, one of which was SLE, where we randomly modified the race (Black/White) and sex (female/male) of the “case” (Fig 1). Primary outcomes were correct text-based responses for SLE diagnosis after initial case presentation (top three initial diagnoses) and after reviewing additional lab results (final diagnosis). We secondarily measured participants’ review time and planned next steps (treatment, referral, tests) as a proxy for certainty. We calculated descriptive statistics for all outcomes (mean, median, proportion) stratified by assigned randomized factor and used chi-square tests to evaluate between group differences with respect to correct diagnoses.
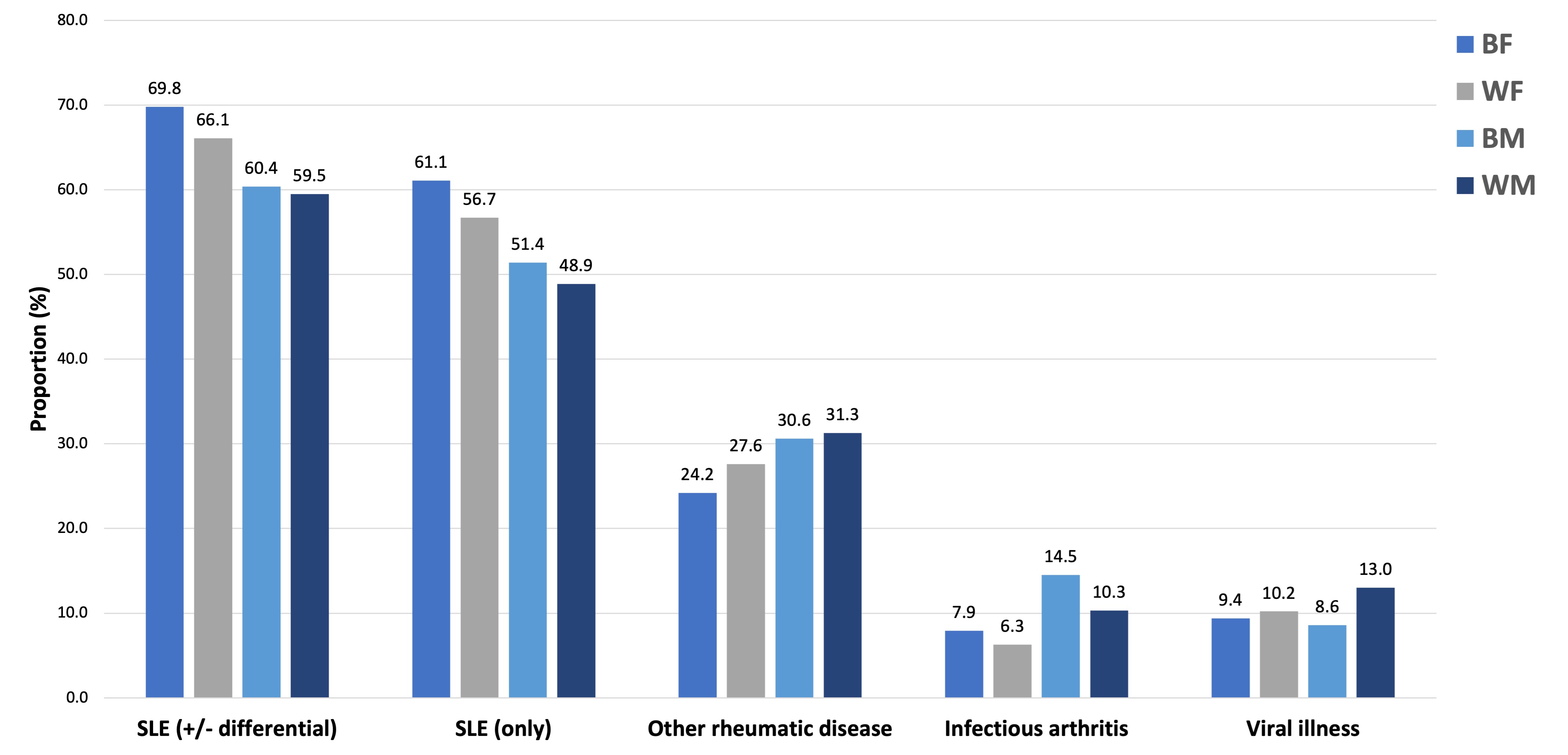
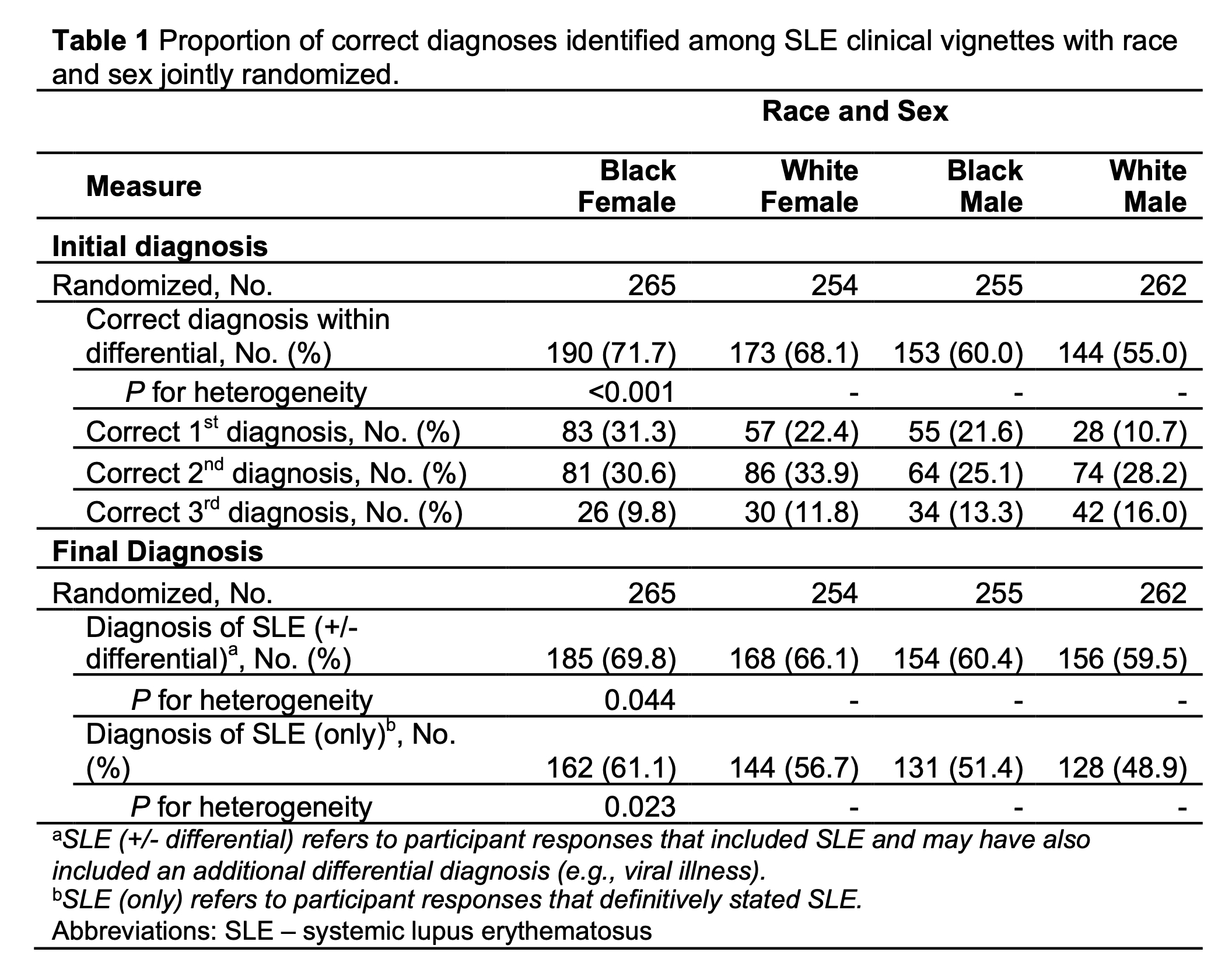
Results: A total of 1036 PCPs (42.6% women, mean age 52.1±12.0 years) completed the survey. Most completed residency ≥11 years ago (76.4%) and indicated their practice focused on patient care (85.6%). At initial case presentation, 63.7% (660/1036) of participants correctly identified SLE within their top three differential diagnoses. These correct initial diagnoses significantly differed according to race and sex, with the highest proportion of correct SLE diagnoses occurring for Black females (Table 1). Overall, most participants elected to order tests (91.8%, 951/1036) and only 7.9% (82/1036) elected to send a referral, of which 95.1% were to rheumatology. Median review time among participants with correct initial diagnoses was longer for White male vignettes (178 s), followed by Black female (154 s), Black male (139 s), and White female (133 s) vignettes. After participants reviewed lab results, the proportion assigning a final diagnosis of SLE (64.0%, 663/1036) remained unchanged from the initial diagnosis. A final diagnosis of SLE occurred more often among female versus male vignettes (Table 1). Infectious arthritis and viral illness were common incorrect diagnoses for Black and White male cases, respectively (Fig 2).
Conclusion: We found that despite identical clinical information, a PCP’s diagnosis of SLE was significantly influenced by the race and sex of the patient. Indeed, the highest accuracy at initial diagnosis occurred for Black females, suggesting cognitive biases in clinical decision-making. These results persisted at the final diagnosis after reviewing additional lab results. Review times also varied by race and sex, with longer times for White males, hinting at varying degrees of diagnostic certainty. Altogether, findings underscore the importance of addressing implicit biases in medical training and practice to ensure equitable diagnostic processes for all patients.
Abbreviations: ANA – antinuclear antibody; CRP – C-reactive protein; ESR – erythrocyte sedimentation rate; PCP – primary care provider; SLE – systemic lupus erythematosus.
Presented diagnoses are for categories that were recorded by ≥5% of participants. Responses for ‘other rheumatic disease’ included rheumatoid arthritis, osteoarthritis, inflammatory arthritis, Bechet’s, and connective tissue diseases. All diagnostic categories aside from SLE (only) are not mutually exclusive.
SLE (+/- differential) refers to participant responses that included SLE and may have also included an additional differential diagnosis (e.g., viral illness).
SLE (only) refers to participant responses that definitively stated SLE.
Abbreviations: BF – Black Female; BM – Black Male; SLE – systemic lupus erythematosus; WF – White Female; WM – White Male
To cite this abstract in AMA style:
Howren A, Tran Q, Sediqi S, Hawa S, Linos E, Falasinnu T, Chaichian Y, Simard J. Beyond the Symptoms: Exploring Cognitive Bias in Lupus Diagnosis Within Primary Care [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/beyond-the-symptoms-exploring-cognitive-bias-in-lupus-diagnosis-within-primary-care/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/beyond-the-symptoms-exploring-cognitive-bias-in-lupus-diagnosis-within-primary-care/