Session Information
Date: Sunday, November 8, 2015
Title: Rheumatoid Arthritis - Human Etiology and Pathogenesis Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Baseline sIL-2Rα
levels predicted total mortality in both pre-RA and matched CN subjects, in a
preceding prospective cohort study (A&R 2010; 62:S19). Now, the trend of
serum sIL-2Rα levels is analyzed over a 20-year interval between cohort
entry to incident RA onset, in pre-RA and matched CN subjects.
Methods: The community-based cohort (N =
21,061 adults) was enrolled in 1974, yielding 54 new onset RA cases, 3 to 20
(mean 12) years after entry (1977 – 1994). Cohort CN subjects (n = 216) were
matched on 1974 entry criteria (4 CN: 1 pre-RA). Stored (-70ºC) sera were
assayed (ELISA) “blindly”, using R & D Systems high sensitivity kits for:
sIL-2Rα; sTNF-R1; 3 inflammatory cytokines; and 2 acute phase protein
levels. Natural log and z-score transformations were performed on all
continuous baseline assay variables. Matched CN subjects were assigned the
intervals to RA onset, within 54 separate sets. Partial (age-adjusted)
correlations of intervals (X-axis) and baseline serum biomarker levels (Y-axis)
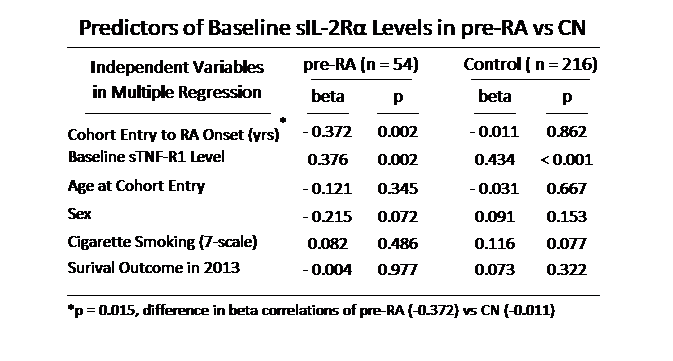
were compared in study groups. Independent predictors of baseline sIL-2Rα levels
(interval from cohort entry to RA onset and other variables of interest) were
identified by multiple regression (MR) models.
Results: Baseline sIL-2Rα and sTNF-R1
levels correlated strongly in total 270 subjects (r = 0.464, p < 0.001) and
in each study group (54 pre-RA, r = 0.473, p < 0.001; 216 CN, r = 0.470, p
< 0.001). In pre-RA, sIL-2Rα levels increased significantly with
decreased interval from 1974 cohort entry to RA onset (r = -0.480, p <
0.001), not found in CN (r = -0.025, p = 0.744), the difference being
significant (p = 0.001) (Fig). In a MR model of pre-RA, baseline sIL-2Rα
levels were significantly predicted by (1) interval (yrs) from cohort entry to
RA onset (beta = -0.372, p = 0.002) and (2) sTNF-R1 levels (beta = 0.376, p =
0.002), but not by: entry age; sex; cigarette smoking; or 2013 survival status.
In 216 CN, sIL-2Rα level was predicted only by sTNF-R1 (beta = 0.434, p
< 0.001), not by the pre-RA interval (beta = -0.011, p = 0.862) or other variables
in the model (Table).
Conclusion: The novel temporal trend of sIL-2Rα
levels may reflect multi-year immunological up-regulation before clinical onset
of RA and deserves further study for confirmation.
To cite this abstract in AMA style:
Masi AT, Rehman AA, Aldag JC, Wang H. Baseline Serum Soluble Interleukin–2 Receptor Alpha (sIL–2Rα) Levels Increased as Intervals Decreased from Cohort Entry to Onset of Incident Rheumatoid Arthritis (pre–RA), not Observed in Matched Control (CN) Subjects [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/baseline-serum-soluble-interleukin2-receptor-alpha-sil2r-levels-increased-as-intervals-decreased-from-cohort-entry-to-onset-of-incident-rheumatoid-arthritis-prera-not/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/baseline-serum-soluble-interleukin2-receptor-alpha-sil2r-levels-increased-as-intervals-decreased-from-cohort-entry-to-onset-of-incident-rheumatoid-arthritis-prera-not/