Session Information
Date: Monday, November 13, 2023
Title: (1013–1032) Healthcare Disparities in Rheumatology Poster II: Socioeconomic Determinants
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients from lower socioeconomic status (SES) backgrounds have low access to total joint arthroplasty (TJA), delays in undergoing TJA, and a higher risk of adverse outcomes compared to those from high-SES backgrounds. The specific barriers to care perceived by patients from lower-SES backgrounds are not well understood, despite the significance of addressing these barriers in reducing disparities in TJA utilization and outcomes. We aimed to assess differences in patient-reported barriers to TJA by patient community poverty level.
Methods: We developed a survey by analyzing interviews with underrepresented minority patients with symptomatic osteoarthritis regarding their concerns about TJA. The 21-question survey assessed five barriers to TJA: 1) trust in surgeon (such as finding a qualified surgeon), 2) recovery (such as lack of social support), 3) cost / insurance (such as concerns about co-pay), 4) fear of poor surgical outcome (such as fear of a future revision), and 5) timing (such as not having severe enough joint pain). Participants indicated whether a barrier was important on a 5-point Likert scale, which we then dichotomized so that “Extremely” and “Very” important were defined as “highly important,” and other responses were “not as important.” The survey was distributed to patients at New York City hospitals and nationally via an arthritis support group. Home addresses were geocoded and linked to census tracts; “high-poverty community” was defined as ≥20% of residents in a community living below the poverty level (American Community Survey data). Multiple logistic regression models were used to evaluate adjusted odds ratios (aOR) of community poverty to rating barriers as “highly important“, adjusted for age, sex, Hip Disability and Osteoarthritis Outcome Score (HOOS, JR) and Knee Injury and Osteoarthritis Outcome Score (KOOS, JR).
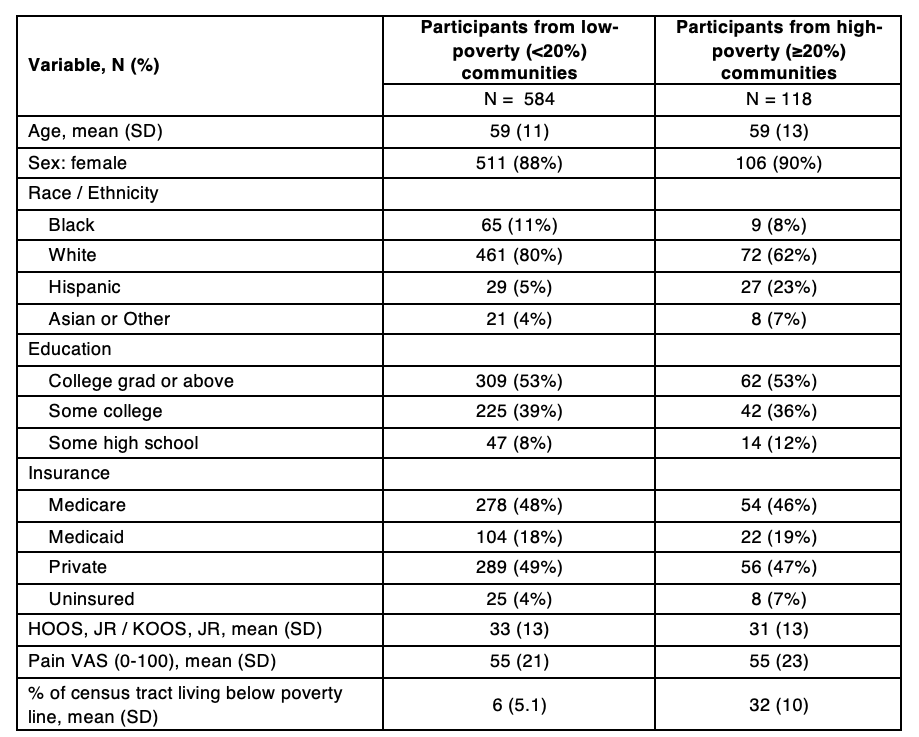
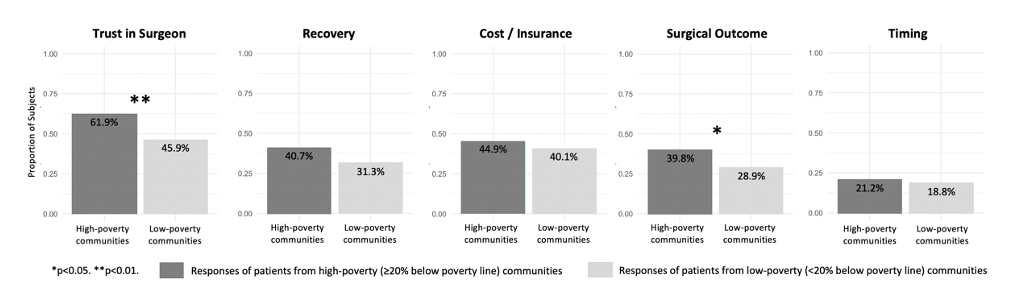
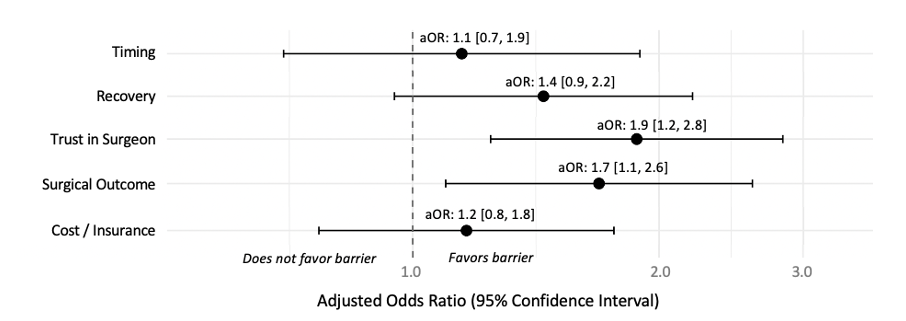
Results: Of the 702 participants who provided an address that could be geocoded, 118 (16.8%) were residents of high-poverty communities (Table 1). Participants from 46 states and Puerto Rico were represented across 658 unique census tracts. All five barriers were more frequently considered “highly important” by residents of high-poverty communities compared to those from low-poverty communities, with differences in surgeon- and outcome-related barriers being the most pronounced (Figure 1). After adjusting for age, sex, and HOOS, JR / KOOS, JR, residents of high-poverty communities had a higher risk of perceiving barriers related to limited or lack of trust in a surgeon (aOR: 1.9, 95% CI: [1.2, 2.8]) and fear of poor surgical outcome (aOR: 1.7, 95% CI: [1.1, 2.6]) as “highly important” (Figure 2).
Conclusion: Residents from high-poverty communities prioritized lack of trust in surgeon and fear of poor surgical outcomes as more significant barriers to TJA compared to residents from low-poverty communities. Our work suggests that facilitating the selection of a trustworthy surgeon and providing education about the process of recovery from TJA among residents from low-income communities could be effective strategies for increasing the uptake of TJA in these communities.
Note: Figures represent N (%) unless stated otherwise. SD = standard deviation. HOOS, JR = Hip Disability and Osteoarthritis Outcome Score. KOOS, JR = Knee Injury and Osteoarthritis Outcome Score. VAS = visual analogue scale.
Note: Models adjust for age, sex, and HOOS, JR / KOOS, JR.
To cite this abstract in AMA style:
Gibbons J, Mannstadt I, Amen T, Rajan M, Young S, Parks M, Figgie M, Bass A, Russell L, Mehta B, Navarro-Millán I, Goodman S. Barriers to Total Joint Arthroplasty for Patients Residing in High-Poverty Communities [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/barriers-to-total-joint-arthroplasty-for-patients-residing-in-high-poverty-communities/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/barriers-to-total-joint-arthroplasty-for-patients-residing-in-high-poverty-communities/