Session Information
Date: Sunday, November 8, 2020
Title: Patient Outcomes, Preferences, & Attitudes Poster II: Miscellaneous Rheumatic Diseases
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatologic conditions are at high risk of hospitalization, ICU admission, and death related to influenza infection due to their underlying diseases and associated treatments. The influenza vaccination rate for the Stanford Rheumatology Clinic during the 2019/2020 influenza season was 61%, leaving a significant number of patients without this protection. We sought to investigate the personal and environmental factors that prevented patients from receiving the influenza vaccine.
Methods: During each clinic visit, patients were asked if they received, plan to receive, or decline the influenza vaccination. At the end of the influenza season, the demographics of patients who received and did not receive the influenza vaccine were compared. Those who did not have a confirmed vaccination in the electronic medical record (EMR) were contacted by secure message or phone and asked open-ended questions regarding their reasoning for not receiving the influenza vaccine in the past year. These responses were recorded and categorized, allowing for multiple responses if given.
Results: Demographic analysis found that patients aged 18-29 were less likely to be vaccinated compared to those aged 50-64 (p=0.018) and those aged 65-79 (p=0.014). No significant difference in vaccination status was found based on sex, race, or health insurance provider (Table 1). Five hundred and ninety two (592) patients without a recorded vaccine at the end of the influenza season were contacted to date and 368 responded (Figure 1). Of those who “Planned To”, 50.3% reported being vaccinated, although this had not been captured in the EMR. The most common barriers cited by this group were lack of time (25.2%) and access (19.4%). In the “Decline” group, patients reported fear of getting sick or side effects (35.6%), belief that they did not need the vaccine (35.2%), and prior negative influenza vaccine experience (25.8%) as reasons for not pursuing vaccination. Only a small proportion reported concerns related to their rheumatologic disease such as prompting a flare (6.1%), a weakened immune system (6.1%), and medication concerns (2.3%). No patient reported cost as a significant barrier.
Conclusion: In patients who desired influenza vaccination, time and vaccine availability were significant barriers. Fear of adverse reaction and prior negative experiences with the influenza vaccine were the primary reasons for active avoidance, although a significant percentage generally did not feel it was necessary. The results of this project can be used for targeted patient education to help improve vaccination rates in the future.
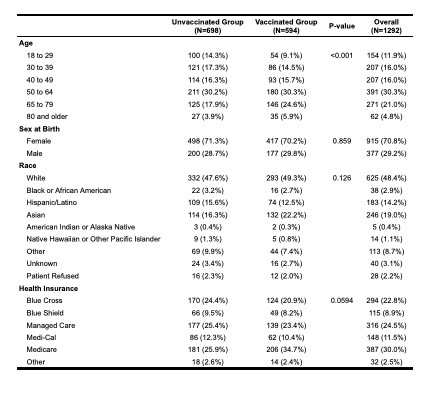 Table 1. Demographics of patients who were vaccinated for influenza during the 2019/2020 influenza season compared to those who remained unvaccinated.
Table 1. Demographics of patients who were vaccinated for influenza during the 2019/2020 influenza season compared to those who remained unvaccinated.
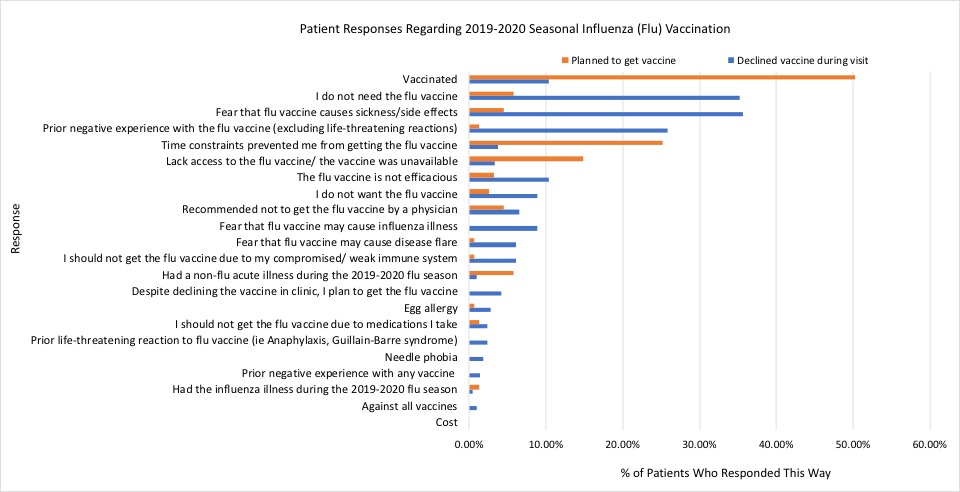 Figure 1. Patient reasons for not obtaining the influenza vaccination during the 2019/2020 influenza season separated into groups of patients who initially planned to get vaccinated (orange, n=155) and declined vaccination (blue, n=213).
Figure 1. Patient reasons for not obtaining the influenza vaccination during the 2019/2020 influenza season separated into groups of patients who initially planned to get vaccinated (orange, n=155) and declined vaccination (blue, n=213).
To cite this abstract in AMA style:
Horomanski A, Triant G, Kolstad K, Dymock M, Lin J. Barriers to Influenza Vaccination in Patients at a Tertiary Care Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/barriers-to-influenza-vaccination-in-patients-at-a-tertiary-care-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/barriers-to-influenza-vaccination-in-patients-at-a-tertiary-care-rheumatology-clinic/
