Session Information
Date: Saturday, November 16, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: A growing arsenal of biologic/targeted synthetic DMARDs often makes inflammation control an attainable target in axial spondyloarthritis (axSpA). Yet, many patients keep suffering from chronic, generalized pain − frequently in its most severe form fibromyalgia (FM) − whereas structured studies of its impact in axSpA are scant. Here, we aimed to estimate the prevalence of thoroughly classified FM in axSpA, explore potential drivers of FM, and study the impact of FM on various disease/health measures, work ability and treatments.
Methods: We included 243 well-characterized axSpA patients from the population-based SPARTAKUS cohort, comprising individuals with both non-radiographic (nr-axSpA; n=78) and radiographic (r-axSpA; n=165) disease. FM was assessed by the 1990 ACR classification criteria. Moreover, patients were evaluated for tender/swollen joints, inflammatory markers, specific axSpA measures (disease activity, physical function, mobility), general patient-reported outcomes, lifestyle factors (BMI, smoking, alcohol use, physical activity), work ability, and treatment history. Potential drivers of FM were cross-sectionally analyzed by logistic regression (FM dependent variable), and variables rather hypothesized to be effects of FM by linear/logistic regression (FM independent variable); crude and adjusted, and with bootstrapped 95% confidence intervals in case of skewness.
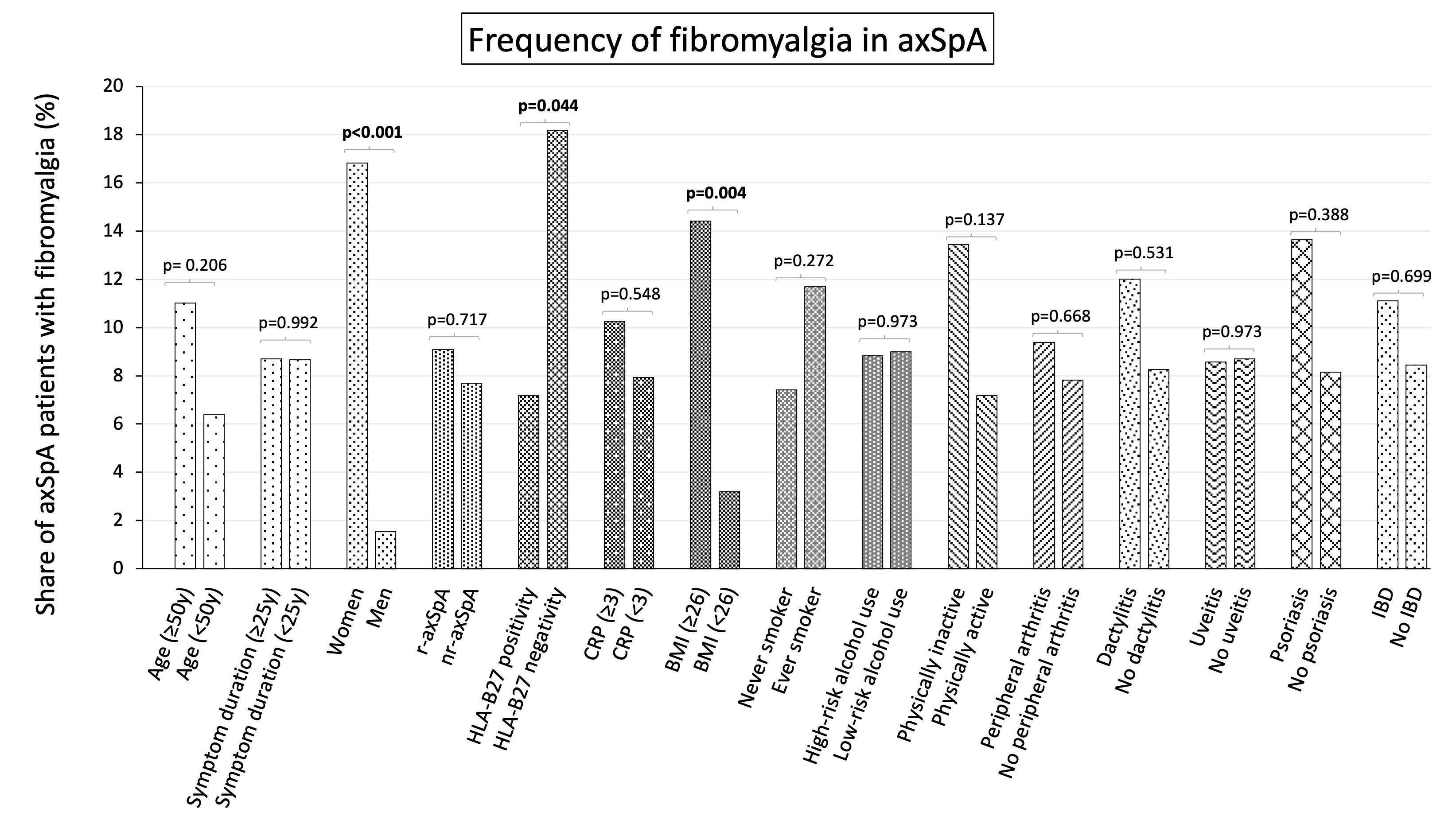
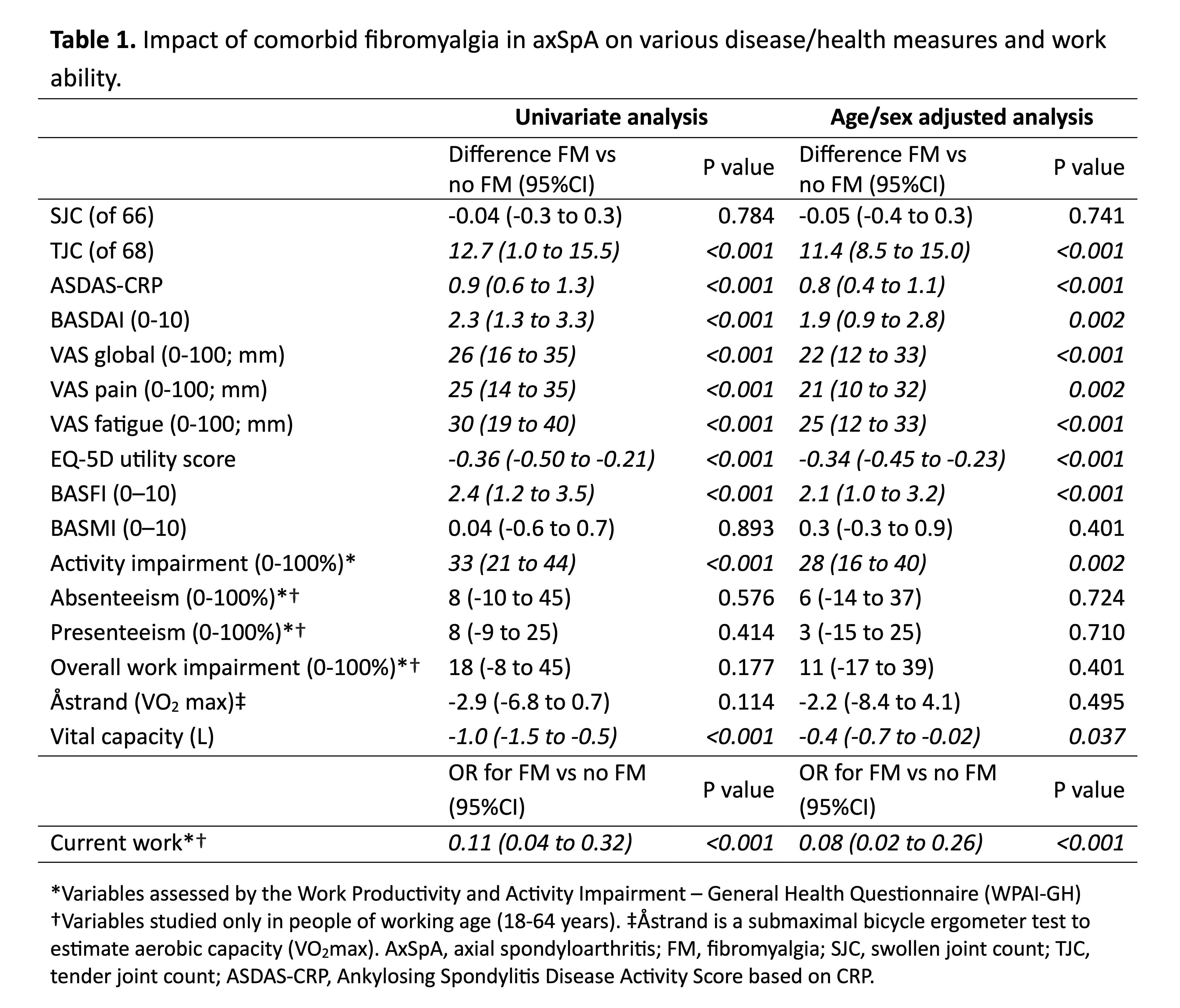
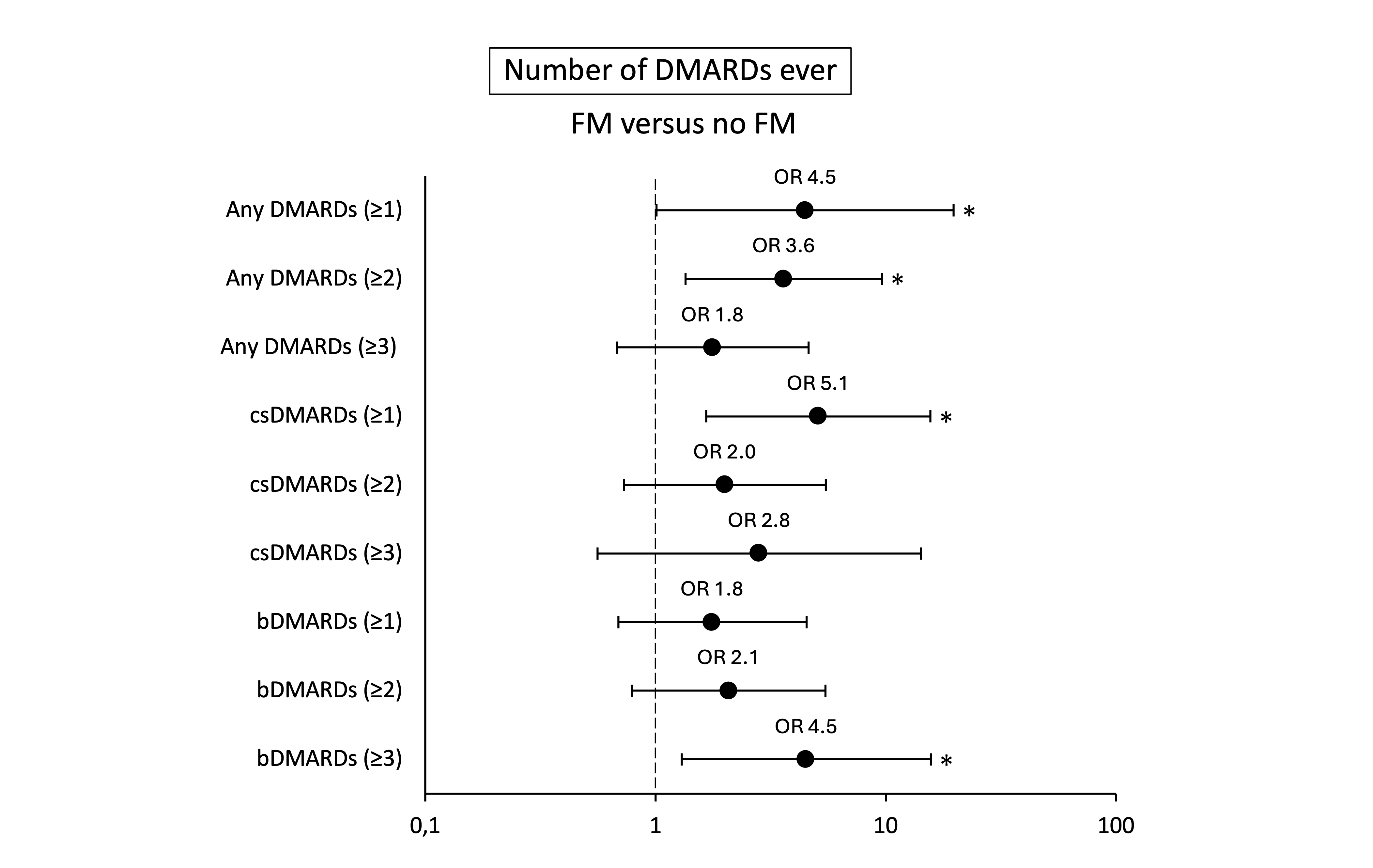
Results: Among the axSpA patients, the proportion of women/mean age/mean symptom duration was 47%/51y/25y. The overall FM prevalence was 9%, with a higher share in female than male patients: 17% vs 2% (crude OR 12.9, 95%CI 2.94–56.9; Figure 1). In crude analysis, FM was also more frequent in patients with higher BMI (OR 1.15, 95%CI 1.05–1.26 per unit increase), and in HLA-B27 negative patients (OR 2.87 95%CI 1.03–8.04 vs positive). Multivariably (including significant variables from crude analysis), only sex and BMI remained significant. No relation to FM status was found for age, symptom duration, axSpA subtype, or CRP level. Regarding the impact of FM, its presence was associated (crude and age/sex adjusted; Table 1) with more tender (but not swollen) joints, worse axSpA disease activity measures (ASDAS-CRP, BASDAI), lower well-being and quality of life (Visual Analogue Scale [VAS] global/pain/fatigue, EQ-5D utility), more functional limitations (BASFI), and lower vital capacity. AxSpA patients with FM also reported more activity impairment and less employment, and were more likely to have received ≥1 DMARD (any) and ≥3 biological DMARDs (Figure 2).
Conclusion: FM is a common comorbidity in axSpA and markedly more frequent in female patients and in those with higher BMI. It is linked to higher disease activity measures, lower well-being and less employment, but not to more objective signs of inflammation. Moreover, axSpA patients with FM have more often tried multiple biological DMARDs, which may reflect difficulties in evaluating axSpA disease activity in the presence of FM. The results underscore a strong negative health impact of comorbid FM and highlight the need for closer monitoring, as well as proper pain-specific pharmacological and non-pharmacological treatments.
To cite this abstract in AMA style:
Brink A, Mogard E, Lindqvist E, Sagard J, Karlsson Wallman J, Olofsson T. Axial Spondyloarthritis Patients with Comorbid Fibromyalgia Feel Worse, Work Less and More Often Try Multiple Biological DMARDs − Results from a Population-Based Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/axial-spondyloarthritis-patients-with-comorbid-fibromyalgia-feel-worse-work-less-and-more-often-try-multiple-biological-dmards-%e2%88%92-results-from-a-population-based-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/axial-spondyloarthritis-patients-with-comorbid-fibromyalgia-feel-worse-work-less-and-more-often-try-multiple-biological-dmards-%e2%88%92-results-from-a-population-based-cohort/