Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Myopathy is an important cause of morbidity in systemic sclerosis (SSc). Nevertheless, scleromyositis remains incompletely characterized owing at least in part to its clinical heterogeneity. Sub-classifying patients with either SSc or autoimmune inflammatory myositis (AIM) by autoantibody profiles is a useful way of identifying more homogeneous subsets. We hypothesized that grouping patients with scleromyositis based on their autoantibody profile would also allow us to identify distinct clinical phenotypes.
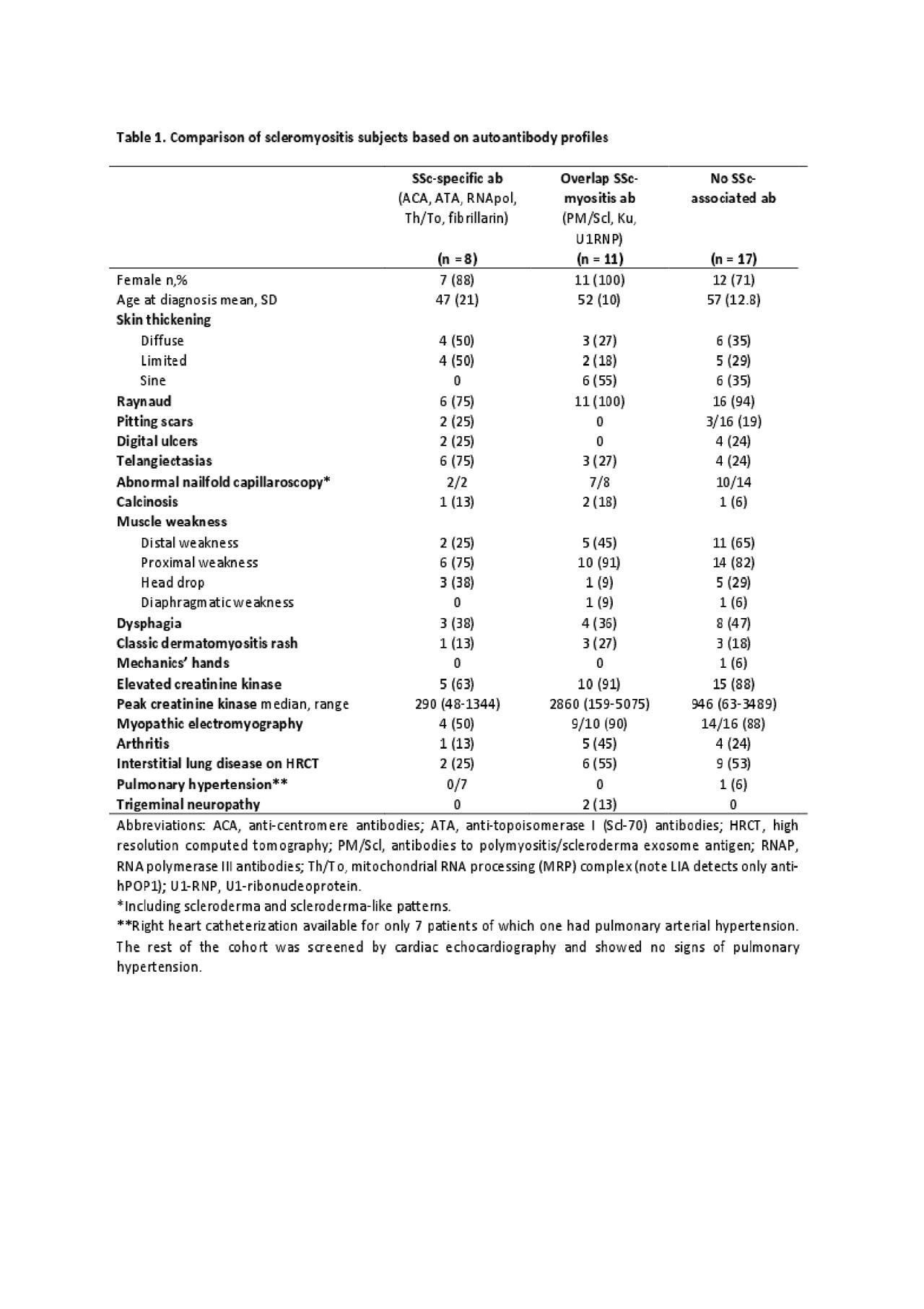
Methods: Thirty-six subjects from a referral centre were identified as having a concomitant diagnosis of SSc and AIM by two rheumatologists. A retrospective chart review was performed and data on demographics, clinical features, laboratory tests and other relevant investigations were extracted. Autoantibodies were assessed by indirect immunofluorescence (IIF) on Hep-2 substrates and line immunoassay (LIA, myositis and systemic sclerosis profiles: Euroimmun, Lübeck, Germany). Subjects were divided into 3 groups based on their autoantibody profiles: group 1 included subjects with SSc-specific autoantibodies (anti-centromere, -topoisomerase 1, -RNA polymerase III, -Th/To, -fibrillarin), group 2 with SSc-overlap autoantibodies (anti-PM/Scl, -U1RNP, -Ku), and group 3 without any fine specificities (hereinafter referred to as ‘seronegative’).
Results: Of the 36 subjects with scleromyositis, 8 (22%) had SSc-specific autoantibodies, 11 (31%) had SSc-overlap autoantibodies and 17 (47%) were seronegative on LIA (Table 1). However, 14 (82%) of the seronegative subjects had positive IIF staining: 6 nuclear speckled and cytoplasmic; 5 nuclear speckled; 2 cytoplasmic; and 1 nucleolar. Most of the subjects were women (83%), had Raynaud’s phenomenon (92%), and abnormal nailfold capillaroscopies (79%). One third of the scleromyositis subjects had no skin involvement and the absence of skin disease was seen more frequently in SSc-overlap and seronegative subjects. Subjects with SSc-specific autoantibodies had lower median creatine kinase (CK) levels (290 IU/L (48-1344)). Subjects with SSc-overlap autoantibodies presented a more classical pattern of weakness associated with significant CK elevation (median (range) 2860 IU/L (159-5075)). Distal weakness was a major feature of seronegative subjects (65%) and head drop was found more frequently in both SSc-associated (38%) and seronegative individuals (29%).
Conclusion: In this carefully phenotyped cohort, autoantibody profiles identified three subsets of scleromyositis associated with distinct patterns of muscle involvement. Just under 50% of subjects had no SSc- or myositis-specific autoantibody identified by LIA, although most of these had positive IIF. Studies are underway to correlate these results with muscle histopathology and to identify novel autoantibodies associated with scleromyositis.
To cite this abstract in AMA style:
D'Aoust J, Leclair V, Gyger G, Meyer A, Fritzler M, Landon-Cardinal O, O'Ferrall E, Karamchandani J, Ellezam B, Massie R, Satoh M, Troyanov Y, Hudson M. Autoantibody Profiles Delineate Three Distinct Subsets of Scleromyositis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/autoantibody-profiles-delineate-three-distinct-subsets-of-scleromyositis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibody-profiles-delineate-three-distinct-subsets-of-scleromyositis/