Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Considering the growing opioid epidemic in the US, it is imperative to have a good understanding of what patient characteristics predict the use of these types of medication. Patients’ attitudes and beliefs about treatments may influence perceptions of need and use of health treatments. Their significance as determinants of utilization of opioid medications for osteoarthritis (OA) treatment is unknown, however. The objective of this study is to determine if patient familiarity with and perceptions of efficacy and risk of opioid medications are associated with opioid medication use for OA.
Methods: Participants with chronic, frequent pain due to knee or hip OA were recruited from a university medical center. A self-administered questionnaire was used to determine use of an opioid medication to treat OA in the last 6 months. The questionnaire also assessed patient familiarity with (3 items, yes/no), and perceptions of efficacy (4 items) and risk (3 items) of opioid medications. Responses to perceptions of efficacy and risk question items were based on a five-category ordinal response scale (score 1-5). Items were averaged, with higher values indicating higher perception of efficacy/risk. Chi-squared or t-tests were conducted to determine if the familiarity and perception of efficacy/risk items were associated with opioid treatment use. Logistic regression was used to determine if observed associations persisted after adjustment for sociodemographic and clinical variables.
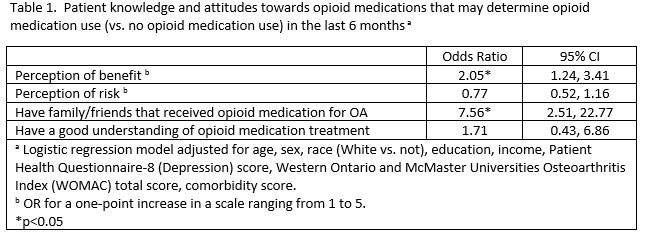
Results: Our sample consists of 100 participants who had used and 249 who had not used an opioid medication for OA treatment in the last 6 months. Users, compared to non-users, were younger (mean age 62.5 vs. 64.8), less likely to have an Associate’s Degree or higher (34.0% vs. 51.0%), and less likely to have ≥$40,000 annual household income (25.5% vs. 45.8%). They also had higher mean WOMAC pain (54.75 vs. 46.76), WOMAC disability (56.64 vs. 44.89), and comorbidity (4.12 vs. 3.23) scores. Opioid medication users were also more likely to have heard about opioids as treatment for OA (95.9% vs. 71.4%), to have family/friends that received a opioid for OA (77.4% vs. 40.4%), and to have a good understanding of what happens after opioid medication treatment (92.2% vs. 64.7%) [all p-values < 0.005]. Mean [SD] perceived efficacy score was higher (3.90 [0.94] vs. 3.27 [0.94], p< 0.005) while perceived risk score was lower (3.20 [1.18] vs. 3.84 [1.07], p< 0.005) among opioid medicine users than non-users. When adjusted for sociodemographic and clinical factors, perception of medication benefit (OR 2.05 [95% CI 1.24, 3.41]) and having family/friends that received the medication for OA (OR 7.56 [95% CI 2.51, 22.77]) remained significantly associated with opioid treatment use (Table 1).
Conclusion: Among patients with knee or hip OA, those who used opioid medications, compared to those who did not, were more familiar with opioids, more likely to believe in their efficacy, and less likely to believe in their risks. Perceived medication efficacy and having family/friends who use the medication were associated with opioid medication use even after controlling for patient sociodemographic and clinical characteristics.
To cite this abstract in AMA style:
Vina E, Dagnino J, Kwoh C. Attitudes and Beliefs About Opioid Medications: Determining Treatment Use in Osteoarthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/attitudes-and-beliefs-about-opioid-medications-determining-treatment-use-in-osteoarthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/attitudes-and-beliefs-about-opioid-medications-determining-treatment-use-in-osteoarthritis/