Session Information
Date: Sunday, November 5, 2017
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment Poster I: Biomarkers and Outcomes
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: A large multicentre multinational inception cohort was established to study risk factors for atherosclerosis (AS) in SLE. We aim to describe all vascular events (VE) and determine the predictors of atherosclerotic vascular events (AVE) in this cohort over a 17 year period.
Methods: Patients enter the cohort within 15 months of SLE diagnosis (≥4 ACR criteria). Clinical and laboratory features of SLE are collected annually in a standardized protocol from 2000-2017. Patients with <3 years of follow-up or VEs attributed to other causes were excluded. VEs recorded include myocardial infarction (MI), angina, congestive heart failure (CHF), intermittent claudication (PVD), transient ischemic attack (TIA), pacemaker insertion and stroke. Diagnosis of a VE is confirmed using standard clinical criteria, relevant laboratory data and imaging where appropriate. Attribution to AS was made on the basis of lupus disease being inactive at the time of VE, and/or the presence of typical AS changes on imaging or pathology and/or evidence of AS elsewhere. Factors associated with AVE were analyzed on patients with AVEs that occurred after study enrollment using time to event analysis with time dependent covariates and cox proportional hazard model.
Results: 1848 patients entered the cohort (88.7%F, age at SLE 34.7 ± 13.4 years, disease duration 5.6 ± 4.2 months, mean follow-up of 7.3 ± 4.5 years). Thus far, there have been 231 VEs in 159 patients. These include: MI (24), angina (31), CHF (52), pacemaker insertion (9), PVD (20), TIA (29) and stroke (66). 106 VEs were attributed to active lupus and 42 to other causes. 83 VE in 57 patients were attributed to AS including: MI (17), angina (26), CHF (12), pacemaker (5), PVD (9), TIA (7), and stroke (7). 14 patients in the AS group had >1 AVE. SLE duration at first AVE was 3.7 ± 3.5 years. Of the 57 AVE patients, 47 had an AVE that occurred after study enrollment.
|
Table 1. Cohort Characteristics at Enrolment |
|
|||||
|
Characteristic |
Patient that had a AVE (N=47) |
Patients that did not have a VE (N=1364) |
p value |
|
||
|
Male |
13 (27.7%) |
133 (9.8%) |
<0.001 |
|
||
|
Caucasian |
34 (72.3%) |
663 (48.6%) |
0.001 |
|
||
|
Age at SLE diagnosis (Mean ± SD) |
51.82 ± 14.89 |
33.99 ± 12.93 |
<0.001 |
|
||
|
Smoking |
25 (53.2%) |
466 (34.2%) |
<0.001 |
|
||
|
Hypertension |
26 (55.3%) |
446 (32.7%) |
0.001 |
|
||
|
Diabetes |
3 (6.7%) |
46 (3.4%) |
0.241 |
|
||
|
Obese |
23 (51.1%) |
381 (28.9%) |
0.001 |
|
||
|
Hypercholesterolemia |
21 (44.7%) |
475 (34.8%) |
0.165 |
|
||
|
Family history of CAD |
21 (45.7%) |
300 (22.5%) |
0.001 |
|
||
|
SLEDAI-2K (Mean ± SD) |
4.13 ± 4.83 |
5.38 ± 5.33 |
0.112 |
|
||
|
Total ACR Criteria (Mean ± SD) Serositis Renal Disorder Neurologic Disorder Immunologic Disorder |
4.96 ± 1.21 21 (44.7%) 12 (25.5%) 3 (6.4%) 39 (83.0%) |
4.91 ± 1.05 367 (26.9%) 389 (28.5%) 55 (4.0%) 1,044 (76.5%) |
0.683 0.007 0.655 0.425 0.304 |
|
||
|
Anticardiolipin |
7/35 (20.0%) |
116/894 (14.5%) |
0.198 |
|
||
|
Lupus Anticoagulant |
13/35 (37.1%) |
187/926 (20.2%) |
0.026 |
|
||
|
Treated with oral steroids |
32 (68.1%) |
928 (69.7%) |
0.802 |
|
||
|
Average daily corticosteroid dose (Mean ± SD) |
14.20 ± 17.58 |
16.73 ± 17.39 |
0.327 |
|
||
|
Treated with antimalarials |
26 (55.3%) |
936 (68.6%) |
0.251 |
|
||
|
Treated with immunosuppressives |
18 (38.3%) |
542 (39.7%) |
0.926 |
|
||
|
Table 2. Predictive Risk Factors – Multivariable Analysis |
||||||
|
Predictor |
Hazard Ratio |
95% Confidence Interval |
p value |
|||
|
Age at SLE diagnosis |
1.08 |
1.06, 1.10 |
<0.001 |
|||
|
ACR Criteria – Serositis |
2.47 |
1.34, 4.54 |
0.003 |
|||
|
Antimalarial treatment |
0.52 |
0.28, 0.95 |
0.033 |
|||
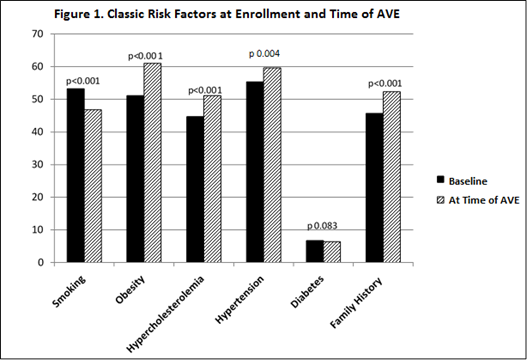
The classic risk factors at inception were not predictive, but they do increase over time (Figure 1).
Conclusion: Over the follow-up of an inception cohort with SLE there were 83 AVEs in 57 patients of which 47 occurred after enrollment. Only older age and serositis are significant risk factors for AVE and antimalarials were protective. However, traditional risk factors increase over time and may have an impact on the development of AVE in the future.
To cite this abstract in AMA style:
Urowitz M, Gladman DD, Anderson N, Su J. Atherosclerotic Vascular Events in a Multinational SLE Inception Cohort: Description and Predictive Risk Factors over a 17 Year Period [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/atherosclerotic-vascular-events-in-a-multinational-sle-inception-cohort-description-and-predictive-risk-factors-over-a-17-year-period/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/atherosclerotic-vascular-events-in-a-multinational-sle-inception-cohort-description-and-predictive-risk-factors-over-a-17-year-period/