Session Information
Date: Sunday, October 26, 2025
Title: (0337–0356) Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: It is well recognized that inflammatory bowel disease (IBD) is associated with osteoporosis and fragility fractures, likely due to multiple factors, including systemic inflammation, corticosteroid use, malabsorption etc. Nonetheless, the exact mechanism for fractures in IBD patients is still unclear. There are multiple studies working with small cohorts, supporting different predictors for fracture risk, yet it remains to be elucidated. This study aims to evaluate the association of demographic and various predictors with fracture risk in IBD patients on and off steroids.
Methods: A retrospective observational study was conducted in IBD patients who had a dual-energy X-ray absorptiometry (DEXA) scan done in the North West of England between 2004 and 2019. Data analysed included demographics, family history of fractures, FRAX™ risk factors, total femur BMD, L1-L4 BMD, fat percentages at different sites including total body, abdomen and both femurs. Chi-square tests were used to assess statistically significant associations between categorical variables, while Student’s t-tests were used for continuous variables. Univariate and multivariate logistic regression models were then utilised to identify significant predictors associated with the development of fractures. Results are shown in both Table 1 and 2.
Results: A total of 1827 patients with IBD were analysed, in which 1495 (81.8%) were female. The mean age at DEXA scan was 65.2 (SD 13.17) years. Fractures occurred in 674 (36.9%) patients, including 573 (31.4%) females and 101 (5.5%) males. Patient with fractures had a higher fat percentage in total, abdominal and femoral regions. Fractures were also associated with lower BMD at all measured sites including L1-L4, femoral necks and total femur.Of the 1252 (68.5%) patients not using steroids, 501 (40.0%) reported fractures, while 88 (24.1%) of the 361 current steroid users had fractures. 65 (44.5%) of the 146 (8.0%) patients with rheumatoid arthritis also reported fractures. 64 out of the 647 patients with fractures reported previous fractures.The multivariate model identified abdominal fat percentage, both right and left femur fat percentages, dual femur fat percentages, both right and left total femur BMD, to be significant predictors of fractures in IBD patients. The right femur fat percentage showed a wide confidence interval (OR 36.40, 95% CI: 1.13–1170.67, p = 0.042), possibly due to sample variability or multicollinearity, though the association remains statistically significant and may be clinically relevant.
Conclusion: Our study showed that lower total femoral BMD is associated with an increased fracture risk in patients with IBD, reinforcing the association between reduced BMD and higher fracture likelihood. Moreover, higher fat percentages in both femoral regions elevate fracture risk, suggesting that body fat composition at different sites may play a role in the development of fragility fractures. It is notable that fractures occurred in a significant proportion of steroid-naive patients with IBD, suggesting that IBD itself contributes to the development of fragility fractures.
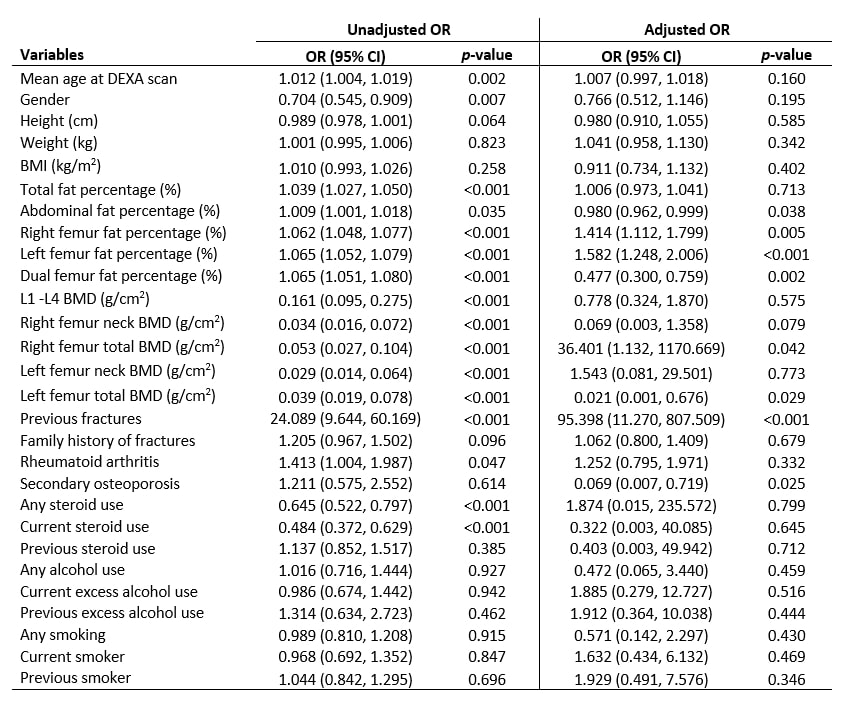 Table 1. Baseline Characteristics of IBD patients
Table 1. Baseline Characteristics of IBD patients
.jpg) Table 2. Univariate and Multivariate model analysis for predictors of fracture in IBD patients
Table 2. Univariate and Multivariate model analysis for predictors of fracture in IBD patients
To cite this abstract in AMA style:
Choy C, Amin H, Bukhari m. Associations with fragility fractures in a population with inflammatory bowel disease (IBD): An observational study. [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/associations-with-fragility-fractures-in-a-population-with-inflammatory-bowel-disease-ibd-an-observational-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-with-fragility-fractures-in-a-population-with-inflammatory-bowel-disease-ibd-an-observational-study/
