Session Information
Date: Saturday, November 16, 2024
Title: Abstracts: RA – Diagnosis, Manifestations, & Outcomes I: Breathe: RA-ILD
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Recent rheumatoid arthritis (RA) genome-wide association studies (GWAS) identified 196 risk loci. Polygenic risk scores (PRS) use GWAS summary statistics to aggregate genome-wide genetic risk for a polygenic disease like RA. We hypothesized that higher RA polygenic risk would be associated with earlier RA onset, seropositive RA, and RA-associated interstitial lung disease (RA-ILD).
Methods: We used a large institutional biobank with over 149,000 patients who provided blood samples and electronic health records data. Participants with RA were identified using a validated algorithm and confirmed to meet RA classification criteria by medical record review. Control patients were participants with available genetic data and no administrative codes for RA or other systemic rheumatic diseases. Genotyping was performed using Illumina MEGA and GSA sequencing arrays. The RA PRS was calculated as a linear sum of beta coefficients of statistically significant loci from summary statistics of a recent transethnic GWAS combined with summary statistics from an association study of human leukocyte antigen alleles and RA risk. We examined associations between the RA PRS and RA diagnosis, seropositivity, age at RA onset, and RA-ILD using logistic regression. In a case-only analysis, we stratified RA patients by RA PRS quartile and examined time to RA diagnosis using multivariable Cox regression.
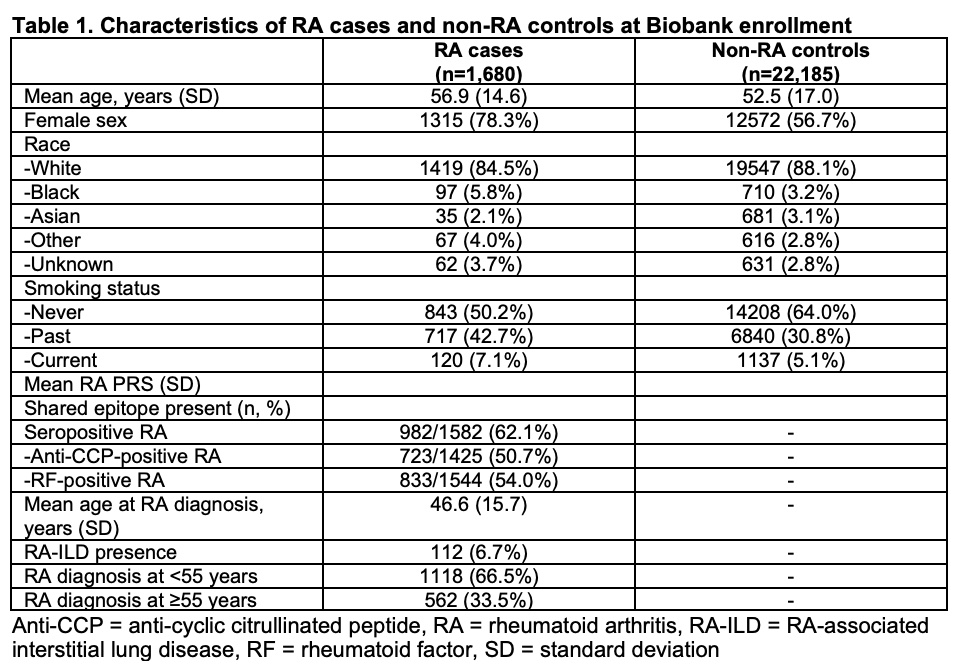
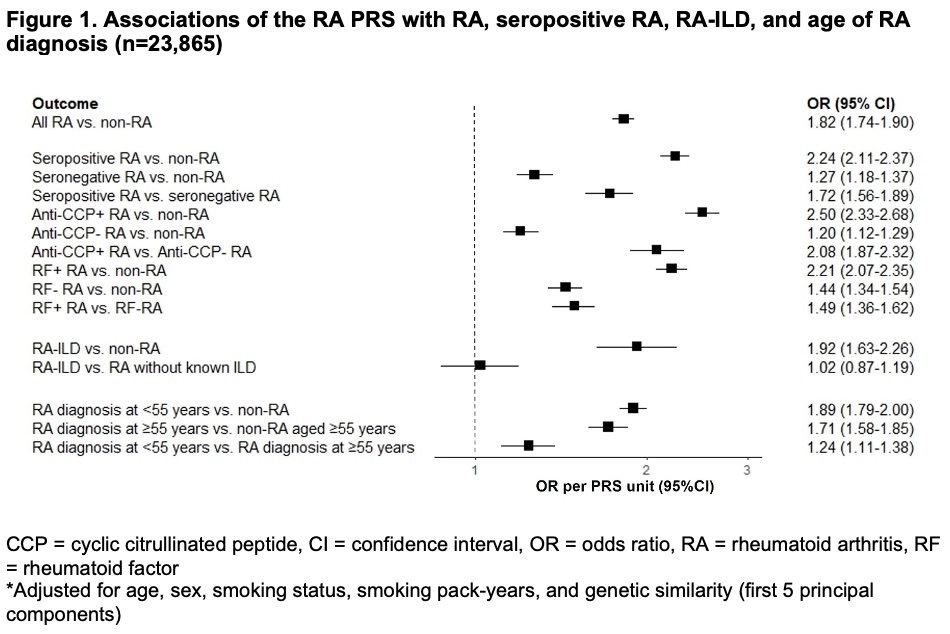
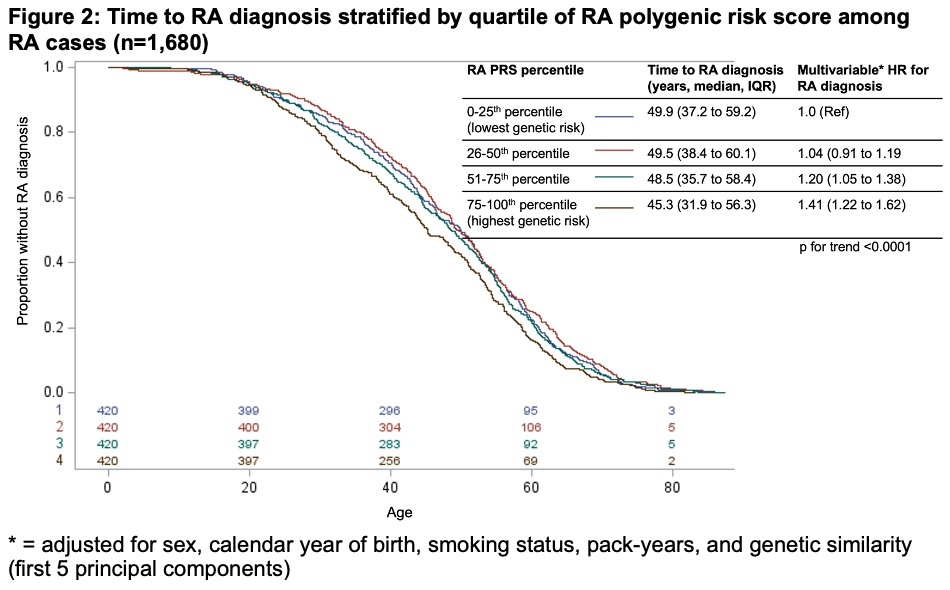
Results: We analyzed 1,680 RA cases and 22,185 non-RA controls. Baseline demographics and clinical RA features for cases are detailed in Table 1. The RA PRS was significantly associated with RA diagnosis (OR 1.82 per unit, 95%CI 1.74-1.90 per PRS unit), seropositive RA (OR 2.24, 95%CI 2.11-2.37), and RA diagnosis before age 55 (OR 1.89, 95%CI 1.79 to 2.00) as detailed in Figure 1. The highest quartile of RA PRS was associated with earlier RA diagnosis (median 45.3 years for highest quartile compared to 49.9 years for lowest quartile) as shown in Figure 2. The hazard ratio for time to RA diagnosis was 1.41 (95%CI 1.22-1.62). Among patients with RA, there were no significant associations between RA PRS and presence of RA-ILD (OR 1.02 0.85 to 1.21).
Conclusion: In a large biobank, the RA PRS was associated with RA diagnosis, earlier-onset RA, and seropositivity. Among patients with RA, higher RA polygenic risk was not significantly associated with RA-ILD. RA patients with the highest quartile of genetic risk had RA onset over 4 years earlier than those in the lowest quartile. These findings serve as a “proof-of-concept” demonstrating that the RA PRS can offer important insights about RA timing and clinical presentation.
To cite this abstract in AMA style:
McDermott G, Juge P, Hayashi K, Wang X, Paudel M, Chang S, Zhang Q, Kronzer V, Mueller K, Saavedra A, Bade K, Qian G, Kowalski E, Vanni K, Cui J, Sparks J. Associations of Rheumatoid Arthritis Polygenic Risk with Age at Onset, Serostatus, and Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/associations-of-rheumatoid-arthritis-polygenic-risk-with-age-at-onset-serostatus-and-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-rheumatoid-arthritis-polygenic-risk-with-age-at-onset-serostatus-and-interstitial-lung-disease/