Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Post-acute sequelae of COVID-19 (PASC, or “long COVID”) is defined by the CDC as COVID-19 symptoms persisting for ≥28 days after infection. Patients with systemic autoimmune rheumatic diseases (SARDs) may be at higher risk for PASC due to their underlying disease and immunosuppressive medications. Disease-modifying antirheumatic drugs (DMARDs), particularly CD20 inhibitors, have been associated with severe COVID-19, but the effect of DMARD use on PASC risk is unclear. Therefore, we investigated the association of baseline DMARD use and PASC among patients with SARDs.
Methods: We invited all SARD patients with COVID-19 within a large healthcare system to participate in a prospective study. Participants completed a survey ≥28 days after confirmed COVID-19 infection, and we analyzed surveys completed from 3/11/2021 to 5/5/2023. The survey collected data on demographics, SARD characteristics, COVID-19 vaccination status, DMARD use at COVID-19 diagnosis, and COVID-19 symptoms and disease course. We categorized DMARD classes by mechanism of action; those taking combination DMARDs were classified by hierarchy of targeted therapy. PASC was defined by any symptom associated with COVID-19 that persisted for ≥28 days. We used logistic regression to estimate odds ratios (OR) for PASC by DMARD class, adjusting for potential confounders.
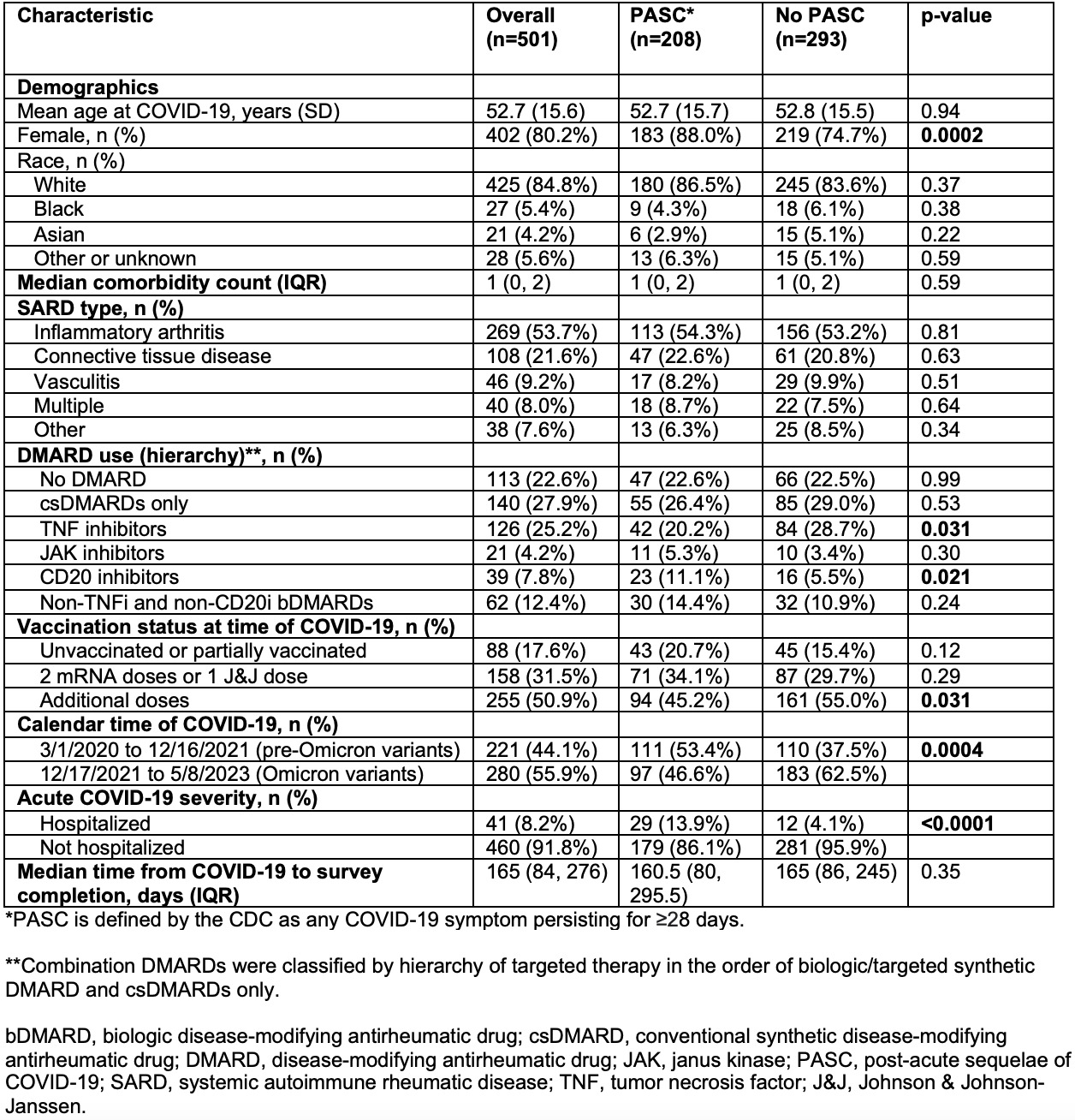
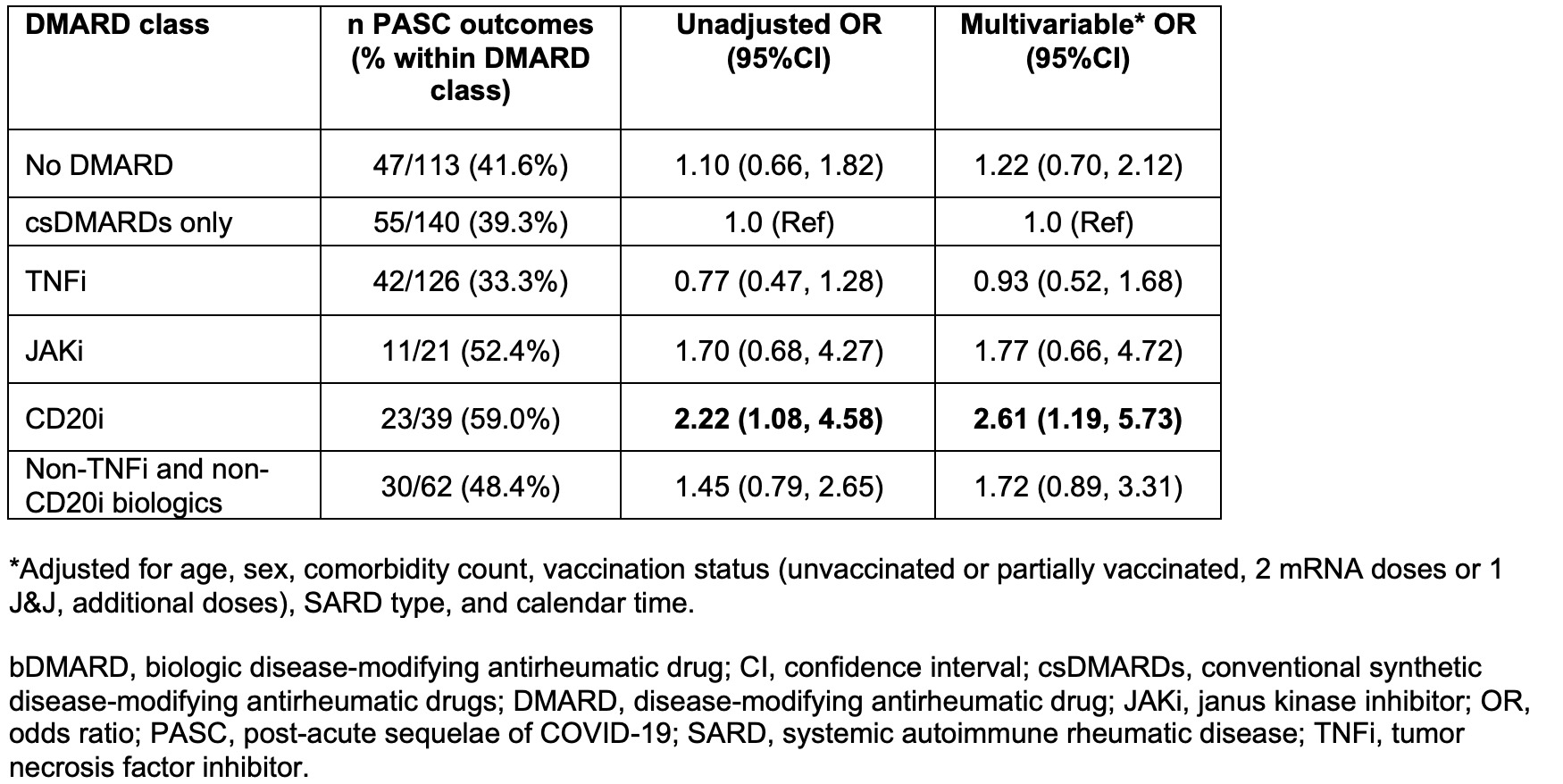
Results: We analyzed 501 patients with SARDs and COVID-19 (mean age 52.7 years, 80.2% female), of which 208 (42%) had PASC. The most common SARD type was inflammatory arthritis (53.7%), followed by connective tissue disease (21.6%). Participants with PASC were more likely to be female (88.0% vs. 74.7%, p=0.0002), less likely to have had additional COVID-19 vaccine doses beyond the primary series (45.2% vs. 55.0%, p=0.031), and more likely to be infected with pre-Omicron variants (53.4% vs. 37.5%, p=0.0004) compared to participants without PASC. Participants with PASC were also less likely to be on TNF inhibitors (20.2% vs. 28.7%, p=0.031) and more likely to be on CD20 inhibitors (11.1% vs. 5.5%, p=0.021). Participants with PASC were more likely to have been hospitalized for COVID-19 (13.9% vs. 4.1%, p< 0.0001). There were no statistically significant differences in age, race, comorbidity count, SARD type, and other DMARD classes, when comparing those with and without PASC (Table 1). After adjusting for comorbidity count, vaccination status, SARD type, and calendar time of infection, SARD patients using CD20 inhibitors had an OR for PASC of 2.61 (95%CI 1.19-5.73) compared to those on conventional synthetic DMARDs (Table 2).
Conclusion: In this prospective study, SARD patients on CD20 inhibitors at COVID-19 onset had increased risk for PASC. This analysis extends previous studies linking CD20 inhibitors with acute COVID-19 severity and suggests vigilance is needed to prevent COVID-19 and monitor for PASC in this vulnerable population. Mechanisms linking B cell depletion with PASC risk may include persistent infection, dysregulated immune response following acute infection, and acute COVID-19 severity from impaired humoral immunity.
To cite this abstract in AMA style:
Venkat R, Wang X, Patel N, Kawano Y, Schiff A, Kowalski E, Cook C, Vanni K, Qian G, Bade K, Saavedra A, Srivatsan S, Williams Z, Wallace Z, Sparks J. Associations of DMARDs with Post-Acute Sequelae of COVID-19 in Patients with Systemic Autoimmune Rheumatic Diseases: A Prospective Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/associations-of-dmards-with-post-acute-sequelae-of-covid-19-in-patients-with-systemic-autoimmune-rheumatic-diseases-a-prospective-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-dmards-with-post-acute-sequelae-of-covid-19-in-patients-with-systemic-autoimmune-rheumatic-diseases-a-prospective-study/