Session Information
Date: Monday, November 14, 2016
Title: Rheumatoid Arthritis – Clinical Aspects II: Risk and Impact of Comorbidity
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: While the impact of interstitial lung disease (ILD) on mortality in RA has been demonstrated, less is known about the influence of other lung diseases either in isolation or in the context of other comorbidity. Thus, we assessed the associations of chronic lung disease (CLD) comorbidity with RA disease characteristics, DMARD use, all-cause mortality, and compared the impact of CLD and cardiovascular disease (CVD) comorbidity on survival.
Methods: Participants were enrollees in a longitudinal observational cohort of US veterans with RA. We characterized comorbidity using the Healthcare Cost and Utilization Project Clinical Classification Software (CLD: categories 127, 128, 130-133; CVD: categories 96-117) from national administrative data over the 12 months preceding enrollment. Analyses were also conducted using ICD-9 codes for ILD and chronic obstructive pulmonary disease (COPD) documented by treating physicians at enrollment. Vital status was determined by the National Death Index. We constructed multivariable logistic and linear regression models to assess associations of CLD comorbidity with RA disease characteristics and medications; multivariable Cox proportional hazards regression models were used to assess the associations with all-cause mortality. Finally, we compared the relative and combined impact of CLD and CVD comorbidity on survival with Kaplan-Meier (KM) curves and Cox regression models.
Results: A total of 2,053 participants were included with mean age of 64 (SD 11) years, RA duration 12 (11) years, 90% male, 87% RF or CCP positive, and 80% current or former smokers. CLD comorbidity was present in 34% (18% COPD, 4% asthma, 2% pleural, 1% external agent/chronic failure, 23% other lung [includes ILD]). CLD comorbidity was associated with higher ESR, CRP, and DAS28 and lower odds of obtaining DAS28 remission (OR 0.76, 95% CI 0.62-0.92). CLD comorbidity was associated with lower odds of ever methotrexate use (OR 0.67, 95% CI 0.55-0.82) and higher odds of ever azathioprine (OR 1.67, 95% CI 1.04-2.67), leflunomide (OR 1.50, 95% CI 1.20-1.87), and prednisone (OR 1.44, 95% CI 1.19-1.76) use. No association was observed with ever biologic use (OR 1.10, 95% CI 0.91-1.34). CLD was associated with 50% increased mortality (95% CI 1.28-1.75), driven by COPD (HR 1.59, 95% CI 1.30-1.94) and other lung disease (HR 1.33, 95% CI 1.24-1.44). Physician classification performed similarly for COPD (HR 1.49, 95% CI 1.18-1.88) but demonstrated increased mortality risk specifically for ILD (HR 1.92, 95% CI 1.26-2.94). KM curves and HRs for CLD and CVD comorbidity are shown in Figure 1.
Conclusion: Chronic lung comorbidity is associated with higher RA disease activity, altered DMARD selection, and increased mortality. Reduced survival is similar, and additive, to that of CVD. Identification and aggressive treatment of chronic lung disease in RA should not be limited to ILD. 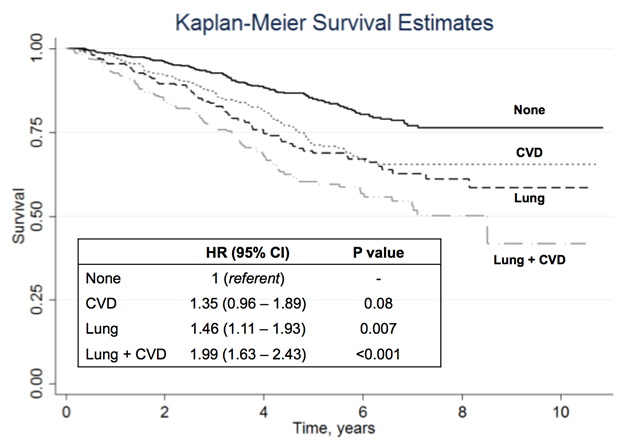
To cite this abstract in AMA style:
England BR, Sayles H, Michaud K, Caplan L, Davis LA, Cannon GW, Sauer B, Solow EB, Reimold A, Kerr GS, Schwab P, Baker JF, Singh N, Mikuls TR. Associations of Chronic Lung Comorbidity with Medications, Disease Activity, and All-Cause Mortality in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/associations-of-chronic-lung-comorbidity-with-medications-disease-activity-and-all-cause-mortality-in-rheumatoid-arthritis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-chronic-lung-comorbidity-with-medications-disease-activity-and-all-cause-mortality-in-rheumatoid-arthritis/
