Session Information
Session Type: Abstract Session
Session Time: 3:15PM-3:30PM
Background/Purpose: Adverse social determinants of health, or social risk factors (e.g., housing instability, food insecurity), contribute to disparities in rheumatic disease care and outcomes. Understanding differences in health care use among individuals with vs. without social risk factors is critical to inform resource allocation, prevention strategies, and outpatient care coordination. We aimed to examine associations between social risk factors and acute care use, including preventable and non-preventable emergency department (ED) visits and hospitalizations, among patients with rheumatic conditions.
Methods: We identified adults ≥18 years with ≥2 ICD-10 codes for a systemic rheumatic condition, inflammatory arthritis, crystalline arthropathy, or osteoarthritis receiving care within a multihospital academic health system, who completed ≥1 social risk factor questionnaire at the time of a rheumatology visit (6/2022-12/2024). We compared the presence vs. absence of social risk factors by demographic factors. Using modified Poisson regression models, we estimated incidence rates (IRs) and incidence rate ratios (IRRs) with 95% confidence intervals for ≥1 ED visit and ≥1 hospitalization following screening among patients reporting ≥1 vs. 0 social risk factor, and by individual social risk factors. We also examined the IR and IRR of preventable ED visits1 by social risk factor presence. Models were adjusted for age, sex, race, ethnicity, primary language, rheumatic condition, and Charlson-Deyo comorbidity index.
Results: Among 9,590 patients with rheumatic conditions screened for social risk factors, 1,614 (17%) reported ≥1 social risk factor. Patients with ≥1 (vs. 0) social risk factor more frequently identified as Black or Hispanic, were ≤50 years of age, spoke Spanish as their primary language, and were Medicaid beneficiaries (Table 1). Among patients with ≥1 social risk factor, 491 (30%) had ≥1 ED visit and 261 (16%) had ≥1 hospitalization following screening. Among patients without risk factors, 1,532 (19%) had ≥1 ED visit and 802 (10%) had ≥1 hospitalization. In adjusted models, there were higher rates of ED visits (IRR 1.38, 95% CI 1.33-1.43) and hospitalizations (IRR 1.59, 95% CI 1.52-1.67) among patients with vs. without social risk factors, and for all individual risk factors except digital access needs (Table 2). Education and transportation needs were associated with the highest rates of ED visits and hospitalizations, respectively. Among patients with any ED visit, 24 (4.9%) of those with risk factors and 63 (4.1%) of those without had ≥1 preventable visit (IRR 1.08, 95% CI 0.92-1.26).
Conclusion: Among patients with rheumatic conditions, presence vs. absence of social risk factors was strongly associated with higher rates of acute care use. The rate of preventable ED visits, however, did not differ. Limitations include inability to adjust for rheumatic disease severity and to account for health care use outside of the multihospital medical system. Future studies are needed to assess mechanisms behind these associations and to test the impact of interventions that address social needs on acute care use. 1 NYU ED Algorithm, https://wagner.nyu.edu/faculty/billings/nyued-background
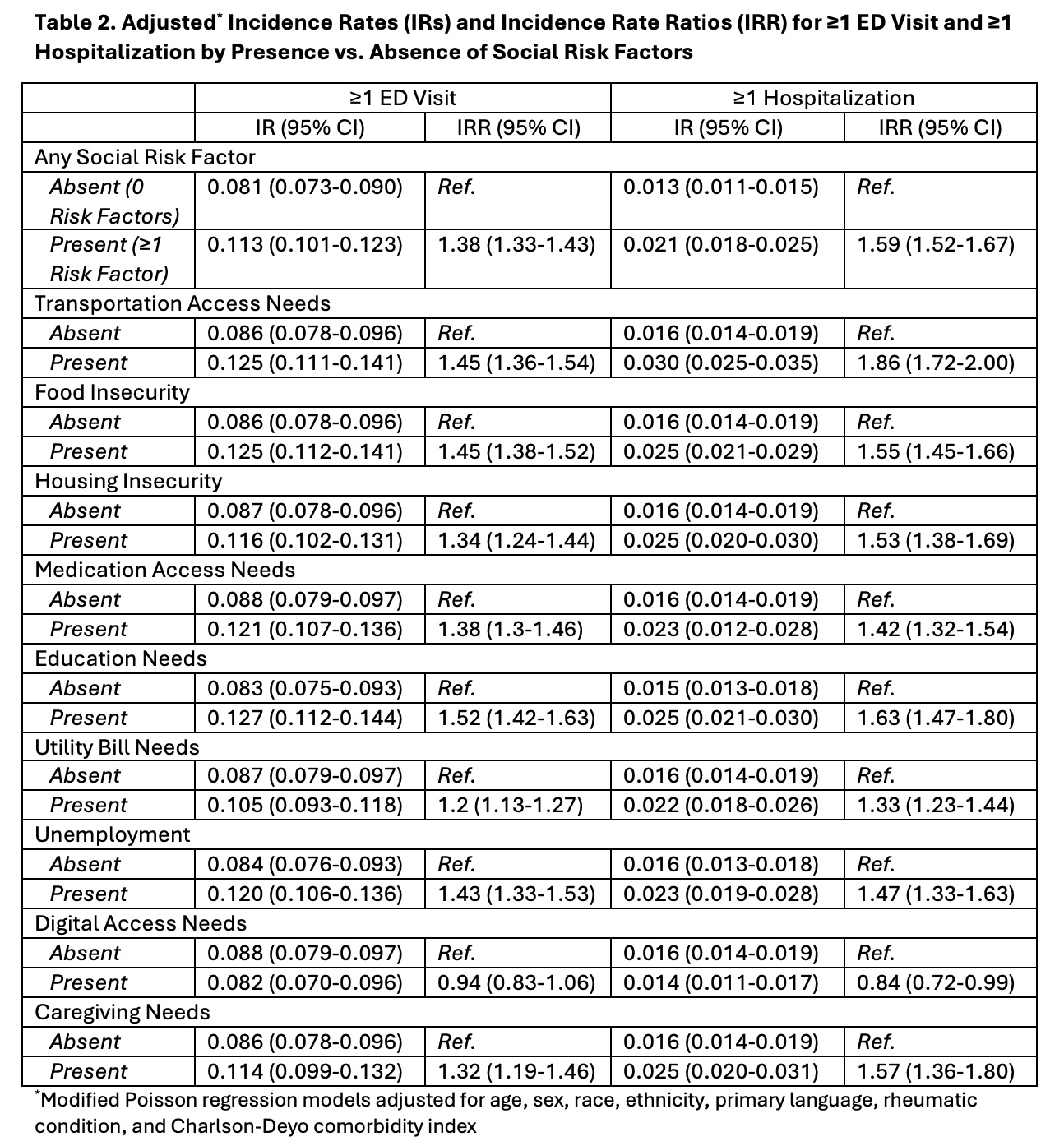 Table 1. Patient Characteristics by Presence vs. Absence of Social Risk Factors
Table 1. Patient Characteristics by Presence vs. Absence of Social Risk Factors
.jpg) Table 2. Adjusted* Incidence Rates (IRs) and Incidence Rate Ratios (IRR) for ≥1 ED Visit and ≥1 Hospitalization by Presence vs. Absence of Social Risk Factors
Table 2. Adjusted* Incidence Rates (IRs) and Incidence Rate Ratios (IRR) for ≥1 ED Visit and ≥1 Hospitalization by Presence vs. Absence of Social Risk Factors
To cite this abstract in AMA style:
Gim H, Santacroce L, Summit R, Retzel K, Bills V, Shadick N, Schoenfeld S, Feldman C. Associations Between Social Risk Factors and Acute Care Use Among Patients with Rheumatic Conditions [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/associations-between-social-risk-factors-and-acute-care-use-among-patients-with-rheumatic-conditions/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-between-social-risk-factors-and-acute-care-use-among-patients-with-rheumatic-conditions/
