Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Adverse social determinants of health (SDoH), or social risk factors like economic insecurities, inadequate health care access and neighborhood vulnerability, contribute to modifiable inequities in rheumatic disease care and outcomes. We examined associations between these factors and rates of acute care use (hospitalizations and emergency department visits) in a national cohort of individuals with systemic lupus erythematosus (SLE), rheumatoid arthritis (RA) and osteoarthritis (OA).
Methods: We included adults (≥18 years) enrolled in the All of Us Research Program with ≥2 ICD-10 codes for SLE, RA or OA ≥2 years prior to enrollment, and SDoH survey responses at enrollment. We developed indices for economic insecurities, health care access challenges, and neighborhood vulnerabilities comprised of counts of social needs reported on the SDoH surveys within each domain. We examined discrimination as an independent social risk factor using the Everyday Discrimination Scale. We determined exposure categories based on data distribution. We measured episodes of acute care use (counts of ED visits and hospitalizations) following All of Us enrollment. We used multivariable negative binomial regression models to examine associations between presence and degree of social risk factor exposure and episodes of acute care use, adjusting for demographic factors, rheumatic condition, and comorbidities.
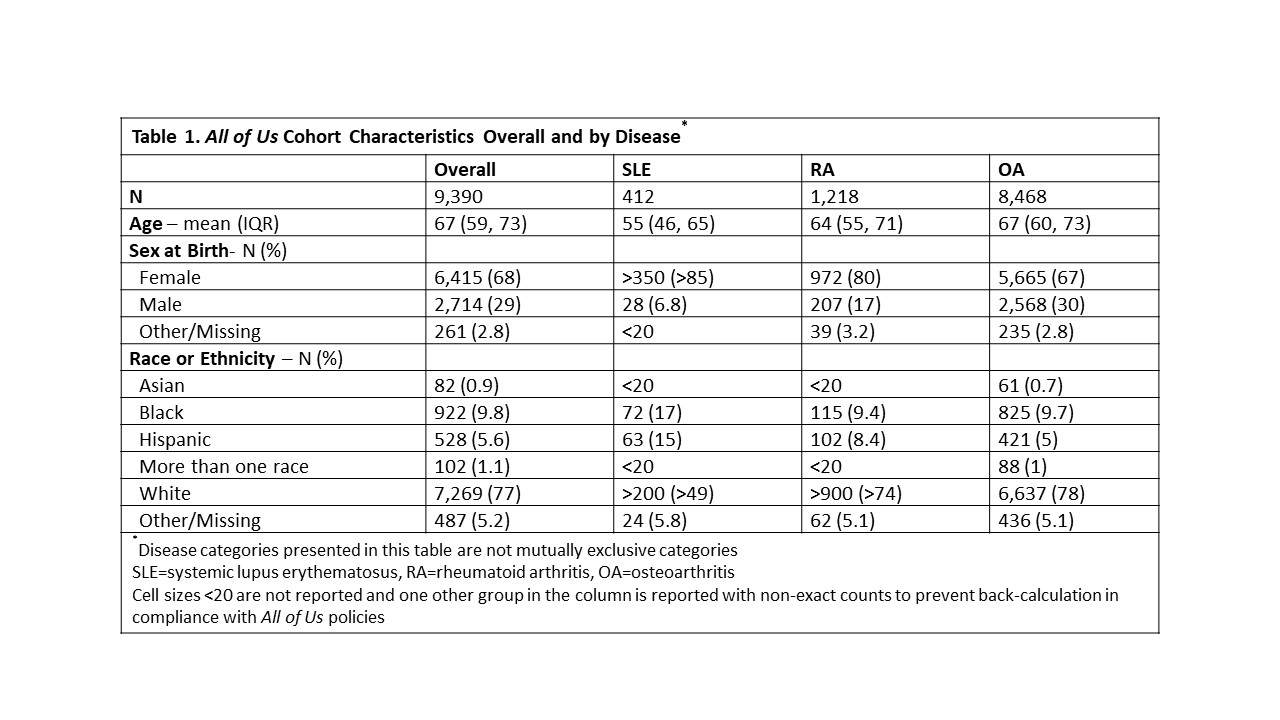
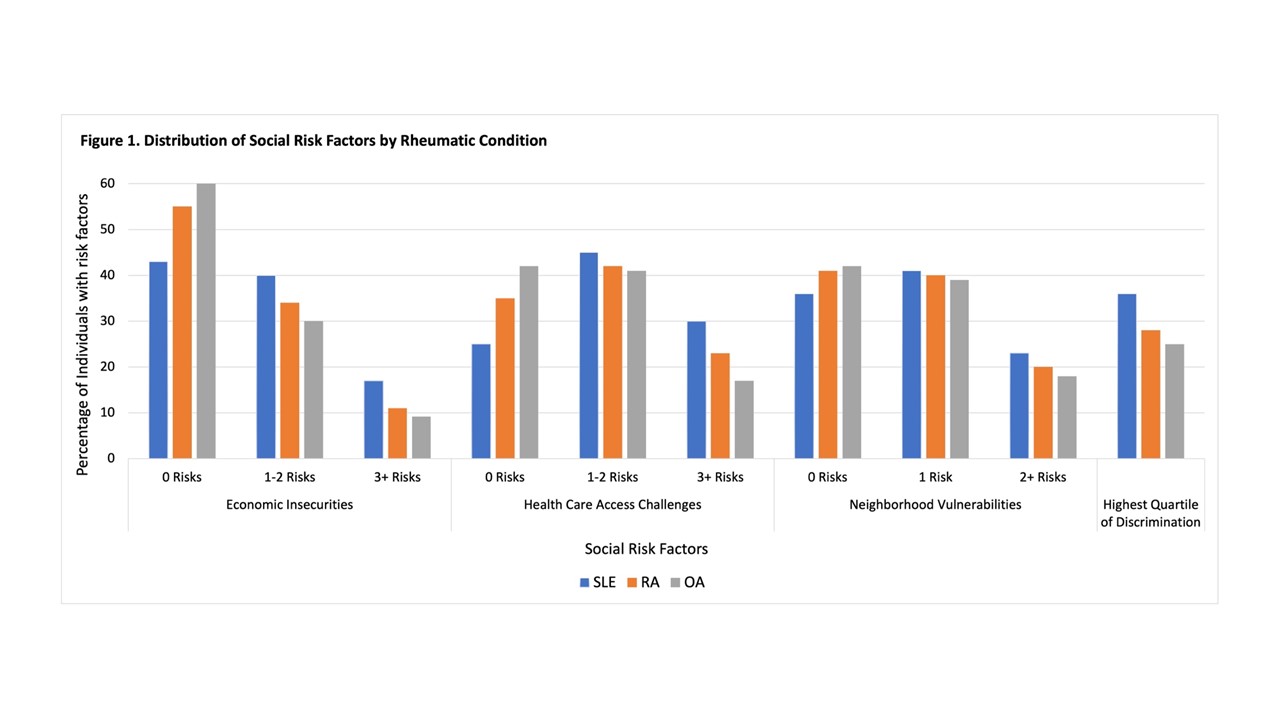
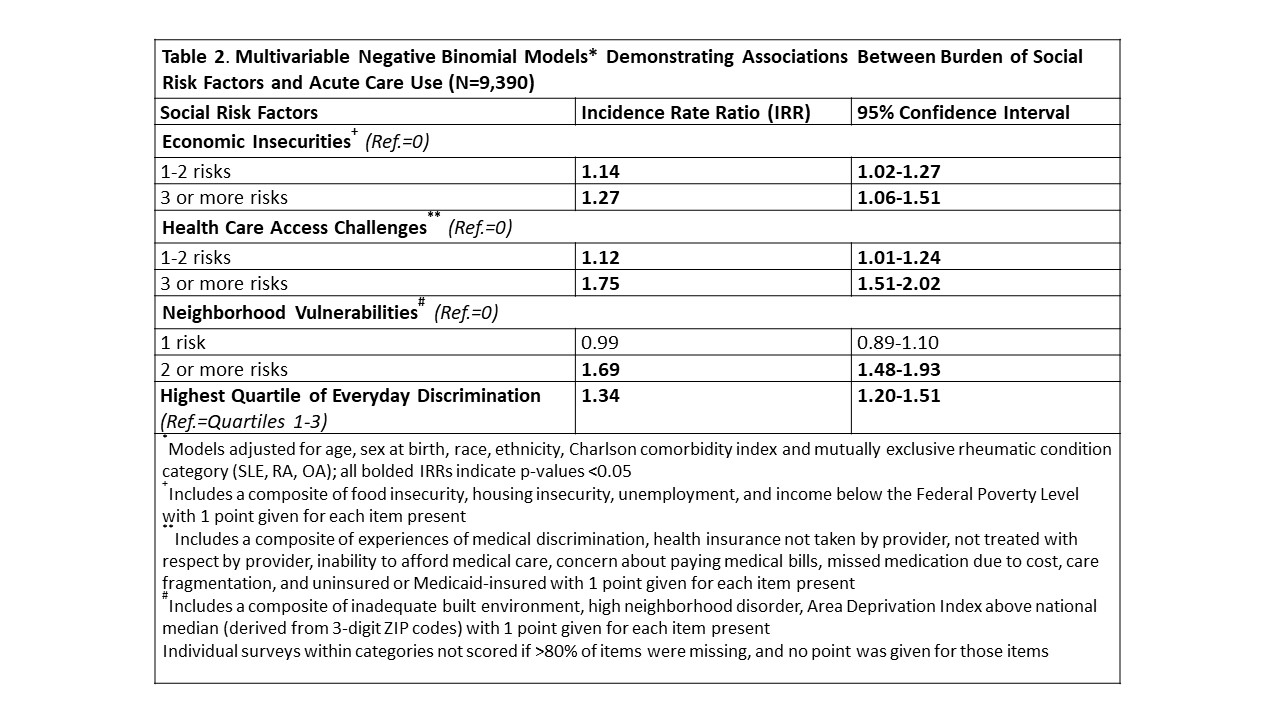
Results: We identified 9,390 individuals; 412 with SLE, 1,218 with RA and 8,468 with OA, and with demographic differences across cohorts (Table 1). The mean (IQR) follow-up time was 4.2 (2.7, 5.3) years, and the mean (IQR) number of acute care events was 3.4 (0, 2). Overall, 40.5% of individuals experienced ≥1 economic insecurity, 59% ≥1 health care access challenge, and 58% ≥1 neighborhood vulnerability, with the greatest burden reported among individuals with SLE (Figure 1). We observed dose-dependent associations between social risk factors and acute care use; greater burden of social risk factors was associated with higher rates of use (Table 2). Repeated experiences of discrimination were associated with significantly higher rates of acute care use, compared to no or less frequent experiences (IRR 1.34, 95% CI 1.20-1.51). The strongest association was seen with ≥3 health care access challenges compared to no challenges (IRR 1.75, 95% CI 1.51-2.02).
Conclusion: In this national cohort of individuals with SLE, RA and OA, we observed a significant burden of social risk factors that were strongly associated with rates of acute care use. Further studies are needed to design and test multilevel interventions to determine whether addressing these needs reduces the profound inequities in rheumatic disease care and outcomes.
To cite this abstract in AMA style:
Feldman C, Santacroce L, Silva Y, Cui J, Yee J, Karlson E, Costenbader K. Associations Between Social Determinants of Health and Acute Care Use Among Individuals with Lupus, Rheumatoid Arthritis and Osteoarthritis in the All of Us Research Program [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/associations-between-social-determinants-of-health-and-acute-care-use-among-individuals-with-lupus-rheumatoid-arthritis-and-osteoarthritis-in-the-all-of-us-research-program/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-between-social-determinants-of-health-and-acute-care-use-among-individuals-with-lupus-rheumatoid-arthritis-and-osteoarthritis-in-the-all-of-us-research-program/