Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Pulmonary arterial hypertension (PAH) is a rare and severe complication of systemic lupus erythematosus (SLE). Human leucocyte antigen (HLA) gene variants in the major histocompatibility complex (MHC) region play key roles in the pathogenesis of SLE. However, the genetic characteristics of HLA in SLE-associated PAH has not been established. In this study, we aimed to identify genetic variants implicated with SLE-associated PAH susceptibility within the MHC region and assessed the contribution of associated variants to clinical outcomes.
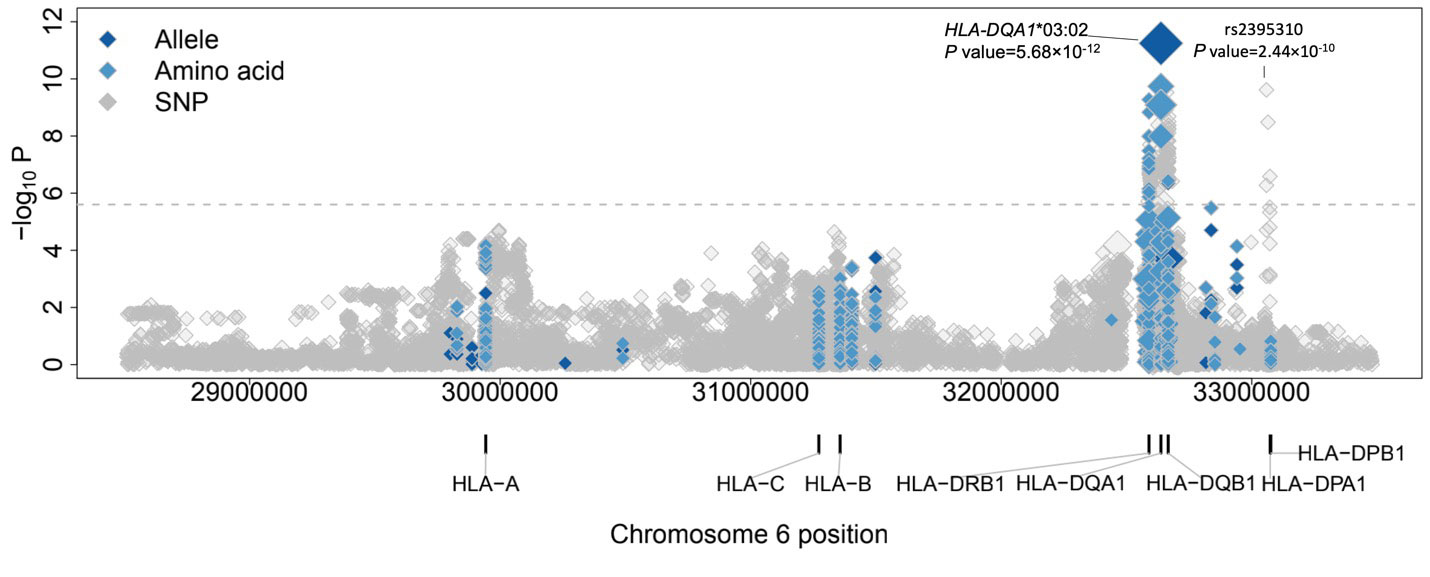
Methods: A total of 172 patients with SLE-associated PAH confirmed by right heart catheterization, 1,303 cases of SLE without PAH and 9,906 healthy controls were included. Deep sequencing was performed on the entire 5-Mb MHC region to identify HLA alleles, single nucleotide polymorphism (SNPs) and amino acid. To determine the HLA genetic variants specifically associated with SLE-associated PAH, we compared it with two groups of controls, which were SLE without PAH (SLE-nonPAH) and healthy controls. Functional analysis were then performed for significant associated SNPs by exploring the evidence of colocalization with expression quantitative trait loci (eQTLs). Finally, we conducted the clinical association study in SLE-associated PAH patients with the significant associated HLA allele.
Results: 19,881 variants were identified, including SNPs, alleles, and amino acid within the MHC region. HLA-DQA1*03:02 was observed presenting the most significant association for SLE-associated PAH when comparing with both healthy controls and SLE-nonPAH. The top significant associated amino acid was mapped to HLA-DQα1 in the region affecting MHC/peptide-CD4+ T cell receptor affinity and antigen binding. Five SNPs were independent detected significantly associated with SLE-associated PAH. Colocalization analysis revealed rs2395310 in HLA-DOA/DPA1 affects the gene expression of HLA-DPA1 and HLA-DPB2 in heart, artery and lung. Clinical association study showed SLE-associated PAH patients with HLA-DQA1*03:02 had worse target role achievement (TGA) and survival rate compared to patients without it.
Conclusion: This is the first study investigating the genetic variants that contribute to SLE-associated PAH susceptibility of the MHC region. HLA-DQA1*03:02 is considered to be a genetic risk factor for the further development of PAH in SLE patients. This HLA allele was also associated with worse clinical outcomes in patients with SLE-associated PAH. SLE patients with this allele type require regular and careful follow-up for early diagnosis and interventions for possible PAH.
To cite this abstract in AMA style:
Qian J, Chen Y, Yang X, Wang Q, ZHAO J, Deng X, Li S, Liu Y, Tian Z, Shen J, Liao Q, Wang Y, Zuo X, Zhang X, LI M, Cui Y, Yu X, Zeng X. Association Study Identified HLA-DQA1 as a Genetic Risk of Systemic Lupus Erythematosus-associated Pulmonary Arterial Hypertension [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/association-study-identified-hla-dqa1-as-a-genetic-risk-of-systemic-lupus-erythematosus-associated-pulmonary-arterial-hypertension/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-study-identified-hla-dqa1-as-a-genetic-risk-of-systemic-lupus-erythematosus-associated-pulmonary-arterial-hypertension/