Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: There is a pathophysiological link between spondyloarthritis (SpA) and Inflammatory Bowel Disease (IBD), so that 10% of IBD is estimated to have SpA and 10% of SpA is estimated to have IBD. Recently, Luchetti et al demonstrated an increased level of bacterial translocation in cases of co-diagnosis of SpA and IBD compared to patients with IBD alone. These data suggest that coexistence of IBD with SpA is associated with more inflammation and therefore more active diseases. The aim of this study is to describe and to evaluate the characteristics of this population in comparison with SpA and IBD alone.
Methods: A single-centre retrospective observational study was conducted. We included all consecutive patients followed between 2019 and 2022 for spondyloarthritis (SpA) meeting the ASAS 2009 criteria and IBD histologically proven. For each patient, we collected demographics, smoking, extrarticular manifestations, imaging data and the number of bDMARDs used. We compare these patients with single diagnosis patients from the MISTIC cohort. The MISTIC cohort, a monocentric cohort, included 2000 patients aged 18–80 years who had SpA, rheumatoid arthritis or IBD and who were regularly followed-up. The MISTIC cohort was approved by the appropriate ethics committee and was conducted according to good clinical practice guidelines. Fischer’s exact test was used for comparison between categorical variables and Student’s t test for quantitative variables.
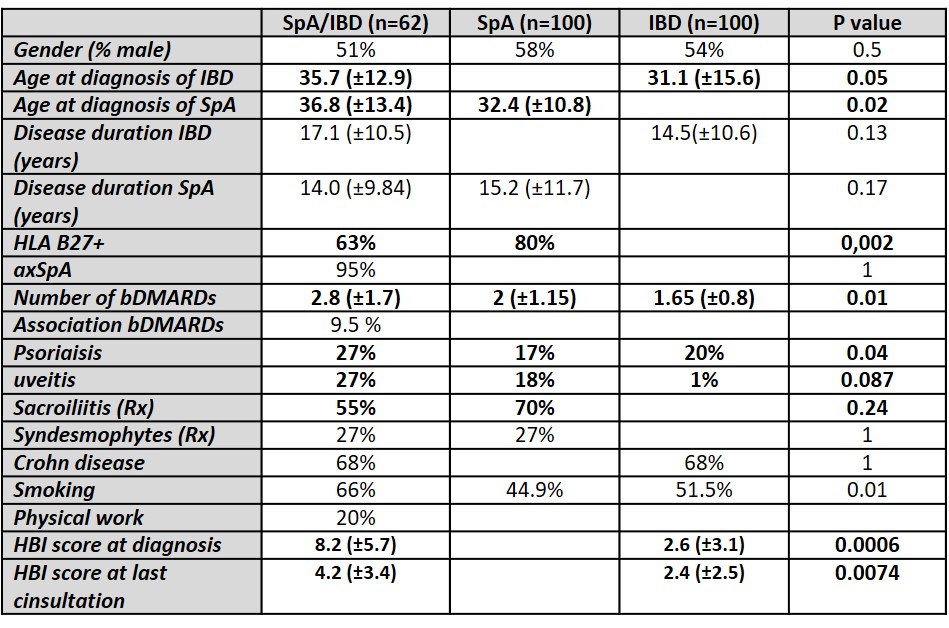
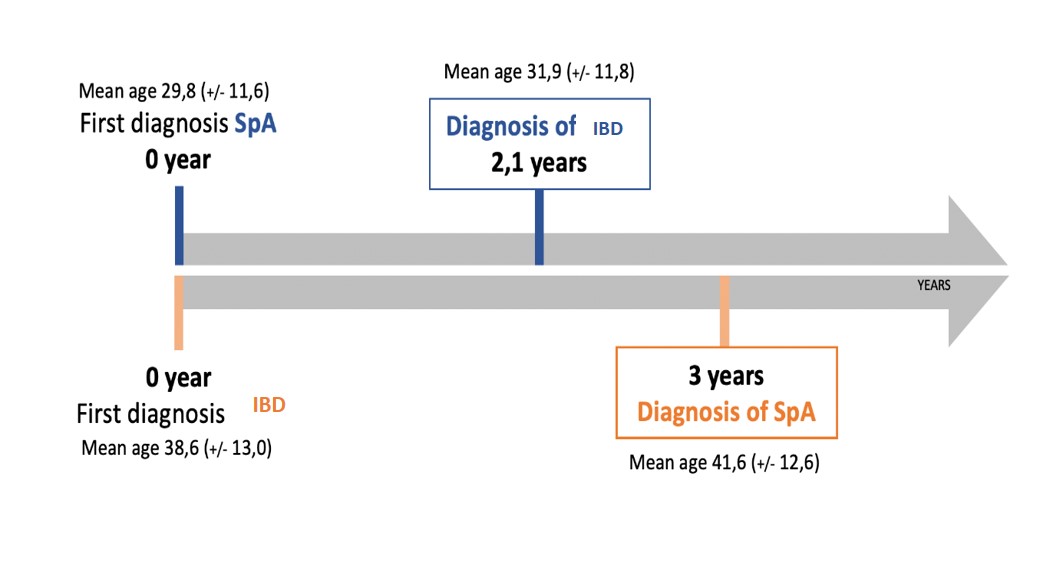
Results: A total of 62 patients with SpA/IBD, 51% male and 67% HLA B27+, were included (table). In 61% of the cases, IBD was diagnosed first, mainly Crohn’s disease (68%), with a mean age at diagnosis of 31.1 (±15.6) years. Concerning SpA, it was mostly axial (95%), with radiographic sacroiliitis (55%) and with a mean age at diagnosis of 36.8 (±13.4) years. Patients had used an average of 3 bDMARDs and 10% were treated with a combination of bDMARDs. When comparing patients with SpA/IBD to those with a single diagnosis of SpA patients were older at diagnosis (36.8 (±13.4) VS 32.4 (±10.8) years old; p= 0.02), had more uveitis (27% VS 18%, p= 0.08) and psoriasis (27% VS 17%, p= 0.04), were more smoker (66% VS 44.9%; p= 0.01) but less HLA B27 positive (63% VS 80%, p= 0.002). They used more bDMARDs for the same disease duration (2.8 (±1.7) VS 2 (±1.15); p= 0.01). When comparing patients with a co-diagnosis to those with a single diagnosis of IBD, patients were older at diagnosis (35.7 (±12.9) VS 31.1 (±15.6) years old; p=0.05), had more uveitis (27% VS 1%, p= 0.08) and psoriasis (27% VS 20%, p= 0.04), were more smoker (66% VS 44.9%; p= 0.01). They used more bDMARDs for the same disease duration (2.8 (±1.7) VS 1.65 (±0.8); p= 0.01). Interstingly, patients with a codiagnosis have a higher endoscopic severity score (HBI) at diagnosis (8.2 (±5.7) VS 2.6 (±3.1) p= 0.0006) and at last follow-up (4.2 (±3.4) VS 2.4 (±2.5); p= 0.0074).
Conclusion: The population of patients with a co-diagnosis of SpA and IBD is a more severe both on the rheumatological and intestinal side. This population showed more frequent extraarticular manifestations and represent a cluster more difficult to treat.
To cite this abstract in AMA style:
Michel J, Prati C, Vuitton L, Toussirot E, Vauchy C, Wendling D, Verhoeven f. Association Spondyloarthritis and Inflammatory Bowel Disease, More Severe Diseases on Both Sides [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/association-spondyloarthritis-and-inflammatory-bowel-disease-more-severe-diseases-on-both-sides/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-spondyloarthritis-and-inflammatory-bowel-disease-more-severe-diseases-on-both-sides/