Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Gait patterns can put stress on the back and weight bearing joints and can even affect upper extremity joints. Walking involves muscle activation and motion across lower extremity, spine, and upper extremity joints. Hence, gait alterations could be related to pain throughout the body. Our objective was to determine whether gait alterations are related to the risk of incident widespread pain (WSP) over 2 years in the Multicenter Osteoarthritis Study (MOST).
Methods: At the 12 year MOST visit (analytic baseline), gait was assessed using inertial sensors (OPAL, APDM, Portland, OR) during a 20-meter walk test at a self-selected speed. At baseline and 2 years later (Year 14 visit), participants reported joints with pain, aching, or stiffness on most of the past 30 days. WSP was considered present if there was pain above and below the waist, right and left sides, and axially. Using data from participants free from WSP at baseline, we used an ensemble machine learning technique (“super learner”) with 8 algorithms to optimally discriminate between persons with and without incident WSP at 2 years. Predictors in the super learner included gait measures, x-ray OA status for each knee, age, sex, BMI, depressive symptoms (CES-D), site, and race (see Table 1 notes). Data were randomly split into 70% training and 30% testing sets. These data splits, i.e., model training and testing steps, were repeated 100 times. We used a variable importance statistic to identify the 10 variables that, across 100 iterations, most frequently contributed to the prediction of incident WSP at 2 years. To quantify the effect of the 10 influential variables selected by the super learner on risk of incident WSP, we used parametric g-computation to estimate marginal risk differences.
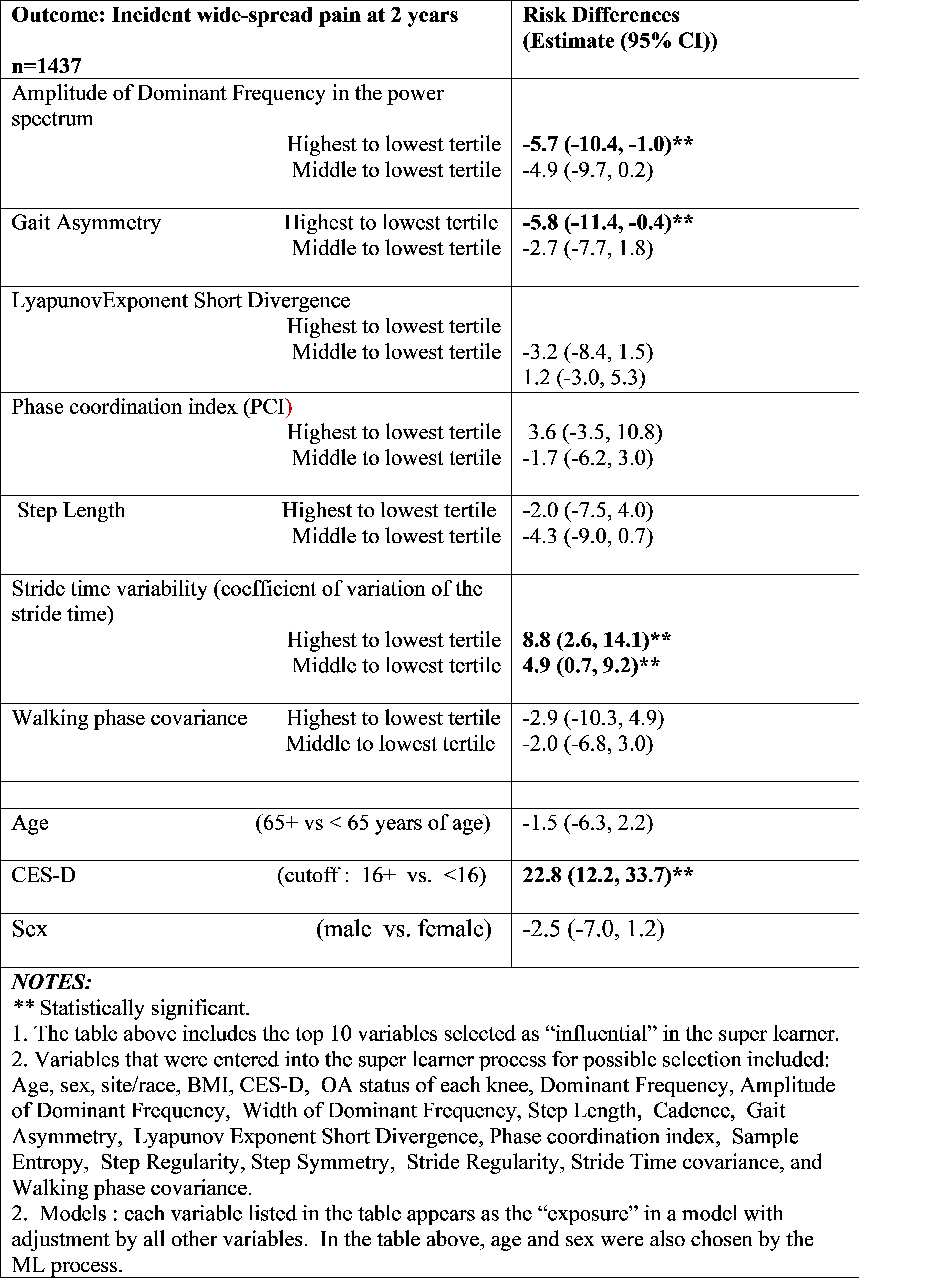
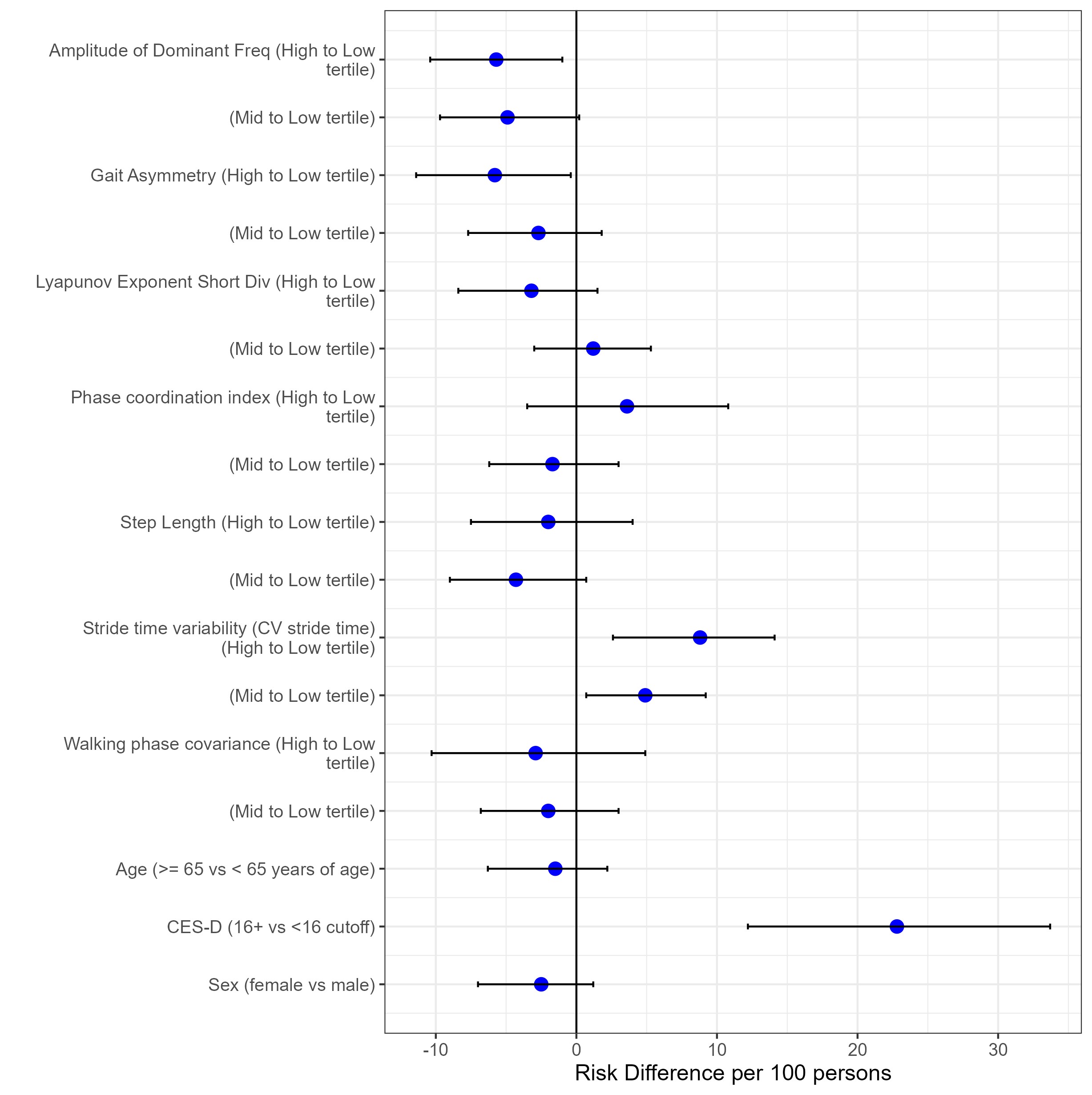
Results: Of the 1437 participants (mean age 63.0[SD: 10.1] years; 56% female) who did not have WSP at baseline, 16.8% developed incident WSP at 2 years. Influential predictors associated with greater risk of incident WSP identified by the super learner (median AUC=0.59) were greater depressive symptoms, greater gait variability (i.e., lower amplitude of dominant frequency, greater stride time covariance) and lower gait asymmetry (Table 1, Figure 1).
Conclusion: We observed that a more variable gait pattern at baseline was related to increased risk of WSP 2 years later. Greater gait variability during standardized walking may reflect an underlying deterioration of neuromotor control of gait and could influence WSP via altered muscle activity and loading across several joints. Gait asymmetry was low in our cohort and hence the clinical relevance of lower gait asymmetry and increased risk of WSP is questionable. Our findings provide novel evidence of a relationship between gait and WSP suggesting that the influence of gait alterations may extend beyond lower extremity joints.
To cite this abstract in AMA style:
Bacon K, Felson D, Jafarzadeh S, Hausdorff J, Gazi E, Segal N, Lewis C, Nevitt M, Kumar D. Association of Wearable-Sensor Derived Gait Measures with Widespread Pain over 2 Years: A Machine Learning Analysis in the Multicenter Osteoarthritis Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-wearable-sensor-derived-gait-measures-with-widespread-pain-over-2-years-a-machine-learning-analysis-in-the-multicenter-osteoarthritis-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-wearable-sensor-derived-gait-measures-with-widespread-pain-over-2-years-a-machine-learning-analysis-in-the-multicenter-osteoarthritis-study/