Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Renal biopsy has long been the gold standard for diagnosis of lupus nephritis (LN), and pathologic features on biopsy are commonly used to guide clinical management. The National Institutes of Health (NIH) activity index (AI) and chronicity index (CI) were developed as a semi-quantitative grading system of pathologic features to allow for more reliable monitoring of LN disease activity and response to treatment. Despite their widespread use, data on the inter-observer reliability and clinical predictive value of the AI and CI have been mixed. In this retrospective cohort study, we aim to evaluate the clinical utility of the AI and CI by assessing their correlation with short and long-term clinical outcomes in patients with biopsy-proven LN.
Methods: This was a single-center, retrospective observational study that included adult patients with systemic lupus erythematosus fulfilling the 1997 revised ACR criteria who had biopsy-proven LN from 1990 to 2020. There were 49 unique patients who underwent 74 renal biopsies during this time period. AI and CI were calculated from biopsy pathology reports and verified by a renal pathologist. Clinical outcome variables including progression to end-stage renal disease (ESRD), serum creatinine, glomerular filtration rate (GFR), and proteinuria (spot urine protein-creatinine ratio or 24-hour urine protein excretion) at 0, 3, 6, 12, and 24 months post biopsy were obtained from chart review. Statistical analysis was performed using analysis of variance/Student’s t-test for continuous parametric variables, Mann-Whitney test for nonparametric variables, and the chi-square test or Fisher’s exact test for categorical variables. Cox hazard regression was used to build models identifying risk factors associated with the time to development of ESRD.
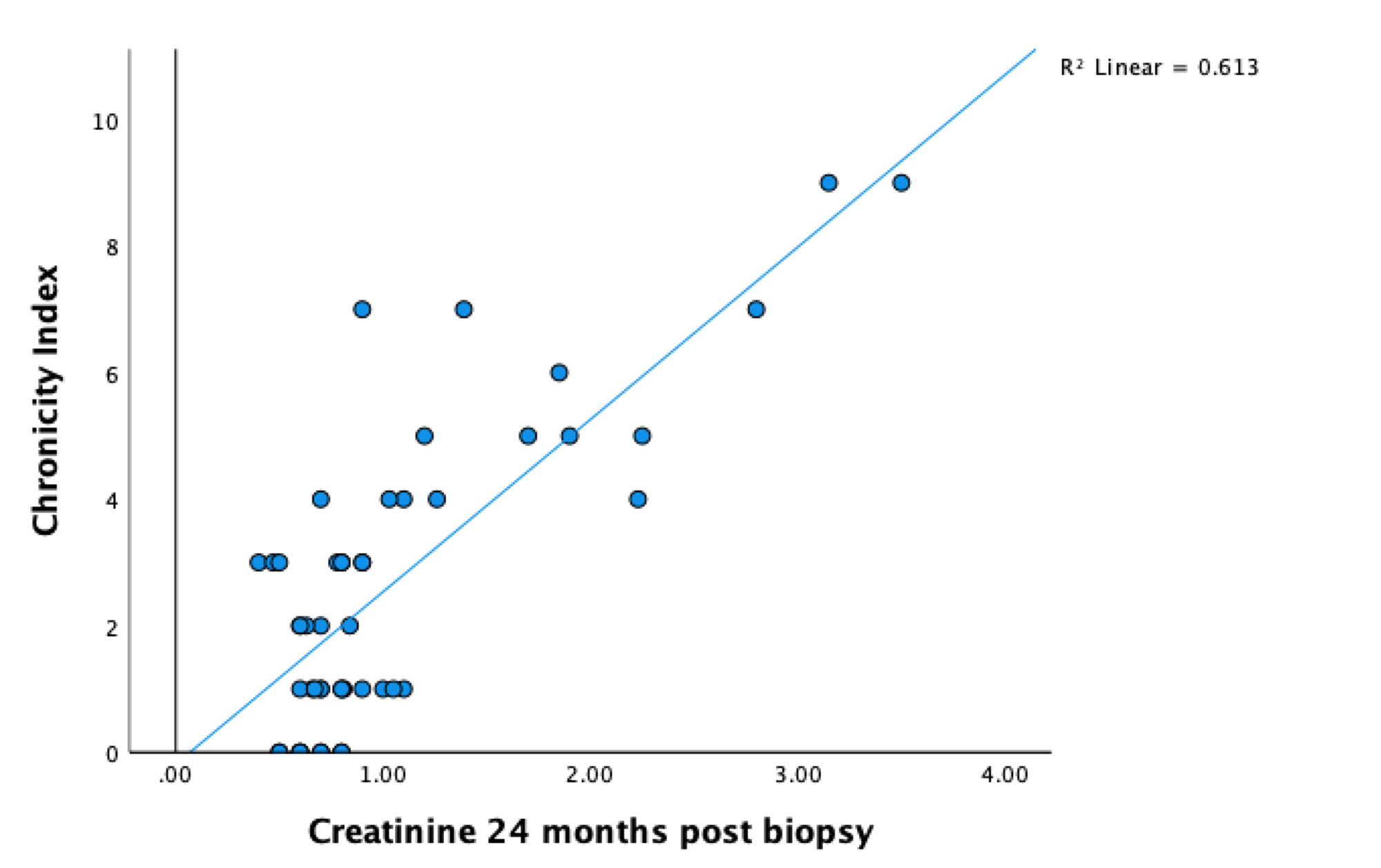
Results: On bivariate analysis, progression to ESRD was significantly associated with higher CI (average CI 4.47 vs. 2.22, p=0.009), while there was a trend towards an association with lower AI (average AI 3.53 vs. 5.40, p=0.15). CI was significantly correlated with serum creatinine and GFR at baseline, 12, and 24 months (figure 1), as well as proteinuria at 12 and 24 months (p< 0.01), but not at baseline. AI was significantly correlated only with proteinuria at baseline (p< 0.01). Based on multivariate Cox hazard regression, CI was a significant positive predictor of time to ESRD (HR=1.497; 95% CI 1.137, 1.971) and AI was a significant negative predictor of time to ESRD (HR=0.785; 95% CI 0.639, 0.965). Baseline serum creatinine and proteinuria were not significant predictors.
Conclusion: Our findings suggest that the CI is a significant predictor of progression to ESRD in patients with LN. Moreover, it correlates significantly with serum creatinine, GFR, and proteinuria at time points as far as two years post biopsy, supporting its use as a marker of chronic and irreversible kidney damage. The AI correlates with baseline proteinuria but not with other clinical markers of kidney function, supporting its use as a marker of acute and reversible kidney damage. Interestingly, the AI is a significant negative predictor of progression to ESRD; the reason for this is not clear and represents an avenue for future investigation.
To cite this abstract in AMA style:
Kellner D, Zuckerman J, Grossman J, McMahon M. Association of Renal Biopsy NIH Activity and Chronicity Scores with Clinical Outcomes in a Cohort of Patients with Lupus Nephritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/association-of-renal-biopsy-nih-activity-and-chronicity-scores-with-clinical-outcomes-in-a-cohort-of-patients-with-lupus-nephritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-renal-biopsy-nih-activity-and-chronicity-scores-with-clinical-outcomes-in-a-cohort-of-patients-with-lupus-nephritis/