Session Information
Date: Tuesday, November 12, 2019
Title: Epidemiology & Public Health Poster III: OA, Gout, & Other Diseases
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The association between periodontal diseases, smoking, and some systemic diseases such as diabetes mellitusis is well established. Periodontitis and rheumatological disorders share common immunological features and there is some evidence of possible association between these diseases. The role of oral dysbiosis from key oral bacteria may play a role in the pathogenesis of autoimmune diseases. This study aims to determine the association between periodontal health and various rheumatic diseases by examining data from the Third National Health and Nutrition Examination Survey (NHANES III).
Methods: The NHANES III is a nationally representative survey of U.S. noninstitutionalized civilians and was conducted from 1988-1994. We included participants aged 13 years and older who had a periodontal examination (Table 1). We used assessments of self-declared physician diagnosis of the following diseases: RA, osteoarthritis (OA), gout, osteoporosis,and systemic lupus erythematosus (SLE). We also included smoking and diabetes mellitus as these have been shown to be significant risk factors for periodontitis. Periodontitis was defined using criteria recommended by the American Academy of Periodontology.
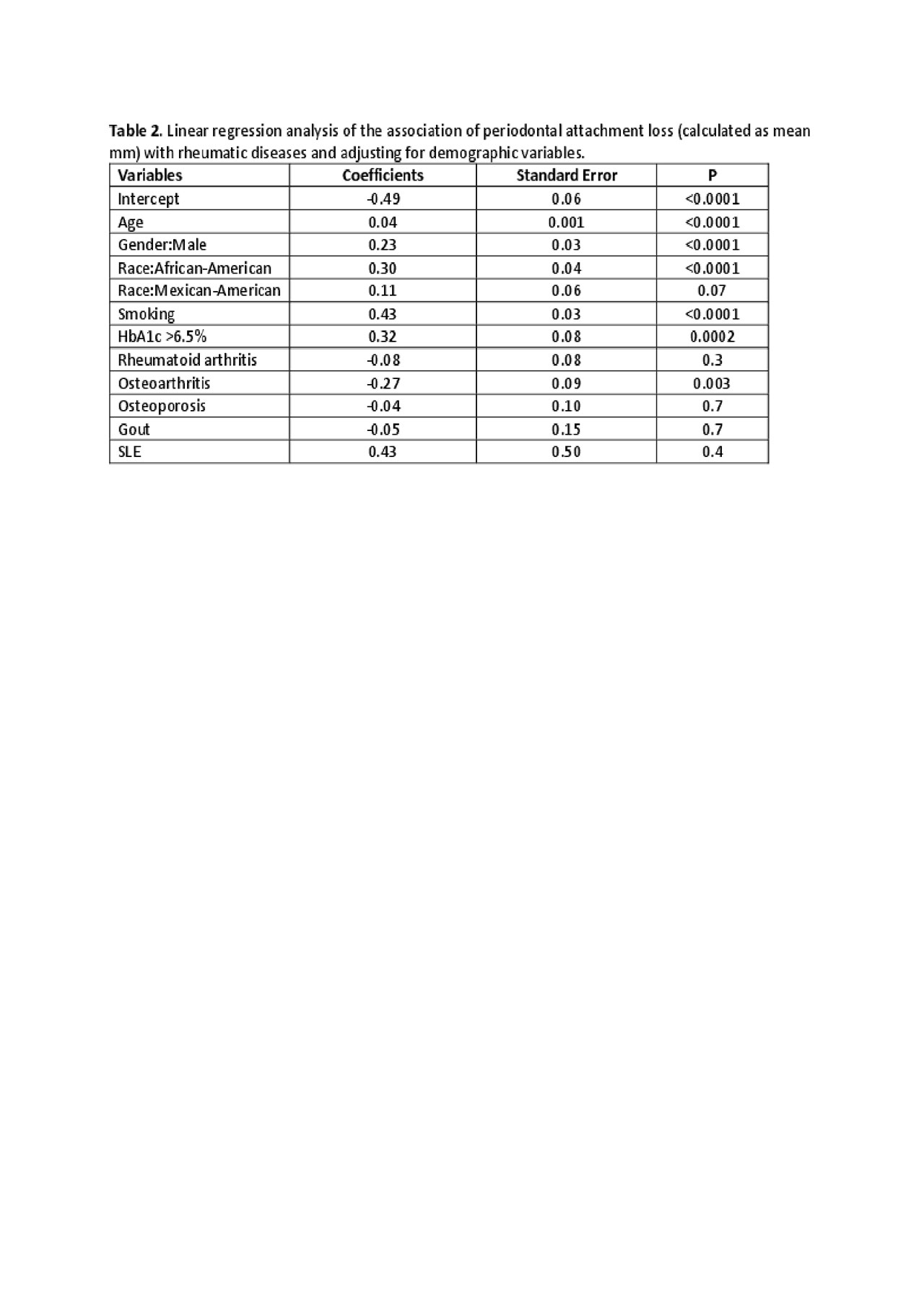
Results: The prevalence of periodontitis and the mean attachment loss increased with age and was significantly higher in males, African-Americans, smokers, and in persons with high HbA1c (Table 2). The regression analysis using mean periodontal attachment loss showed that the association of periodontitis with rheumatic diseases, including rheumatoid arthritis, was not statistically significant except for osteoarthritis (p=0.003). Similarly, using the diagnosis of periodontitis as the outcome variable, the logistic regression model showed no significant relationship between periodontitis and rheumatic diseases, except for osteoarthritis which showed a negative relationship with periodontitis (OR= 0.7, p=0.03), after controlling for the effect of other co-variates (Table 3).
Conclusion: This study shows positive associations of periodontitis with known risk factors, such as demographics, smoking, and diabetes mellitus, but it failed to show statistically significant positive association with systemic rheumatic diseases including RA. This is in contrast with other studies showing positive association of many rheumatic diseases especially RA with periodontitis. There was a trend toward an association of periodontitis with SLE but the number of SLE patients was very small. The negative association between osteoarthritis and periodontitis is unexplained. More prospective studies are needed to confirm or refute the association between periodontitis and rheumatic diseases.
To cite this abstract in AMA style:
Tiwari V, Brent L, Albandar J, Hsiao C, Shah S. Association of Periodontitis with Rheumatological Disorders: NHANES III Analysis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/association-of-periodontitis-with-rheumatological-disorders-nhanes-iii-analysis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-periodontitis-with-rheumatological-disorders-nhanes-iii-analysis/