Session Information
Date: Monday, November 11, 2019
Title: 4M115: Pain Mechanisms – Basic & Clinical Science (1878–1883)
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Despite the availability of potent disease modifying anti-rheumatic drugs (DMARDs), a significant percentage of rheumatoid arthritis (RA) patients do not achieve low disease activity or remission defined by composite disease activity measures (CDAMs). Although CDAMs are intended to reflect inflammation, non-inflammatory processes may also contribute to high scores. For instance, dysregulated central nervous system processing, termed “pain centralization”, is associated with high patient global assessment and tender joint count, both of which are components of CDAMs. The objective of this study was to assess the contribution of pain centralization to DMARD response.
Methods: One hundred and eighty-two RA patients with active disease necessitating DMARD initiation or change were included in this longitudinal prospective multicenter cohort. All patients met ACR criteria for RA. Patients were assessed before and approximately 12-weeks after DMARD initiation or change. The outcome was good response per the European League Against Rheumatism (EULAR) response criteria. Primary predictors were pain centralization assessed by quantitative sensory testing (QST). Overall pain centralization was measured by pressure pain thresholds (PPTs). Pain facilitation was assessed by temporal summation (TS). Impaired pain inhibition was measured by conditioned pain modulation (CPM). The secondary predictor was a combined measure of TS and CPM. Predictors were dichotomized into least central dysregulation and greater central dysregulation using a split between the 1st and 2nd sex-specific tertiles for each QST measure. Multiple logistic regression was used to calculate odds ratios (ORs) for good EULAR response.
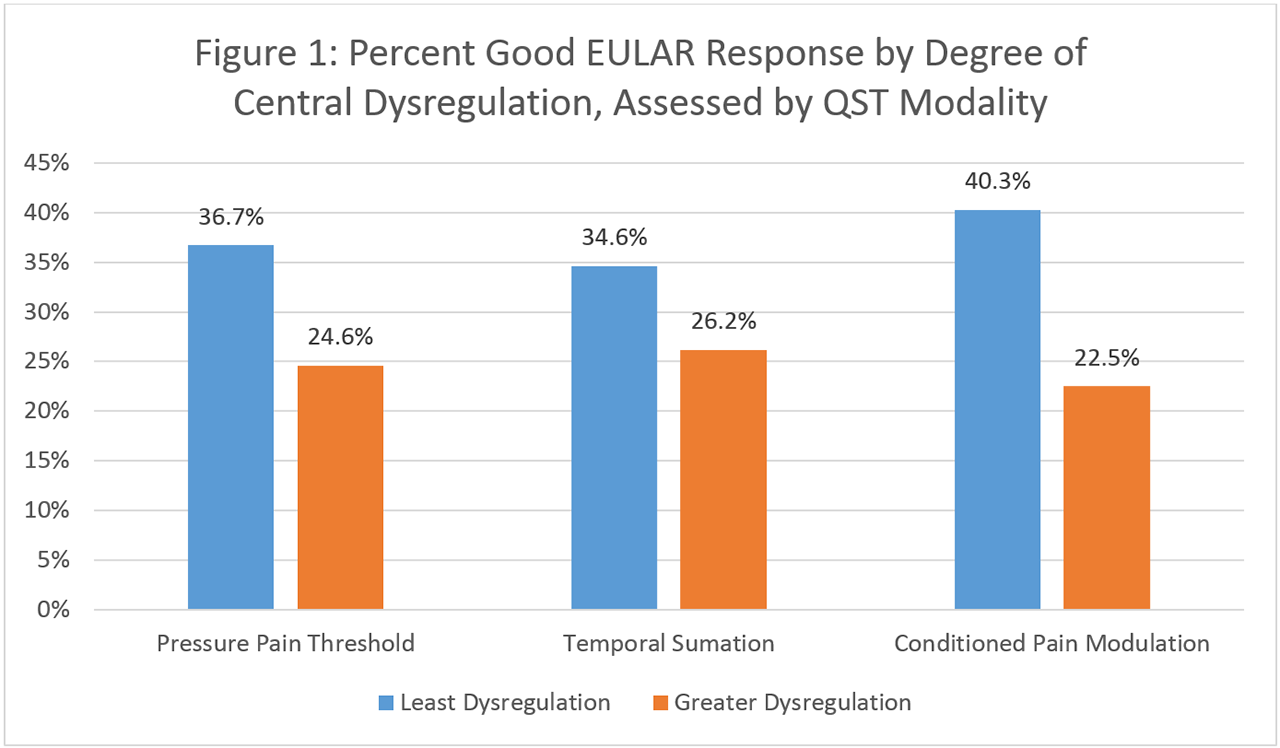
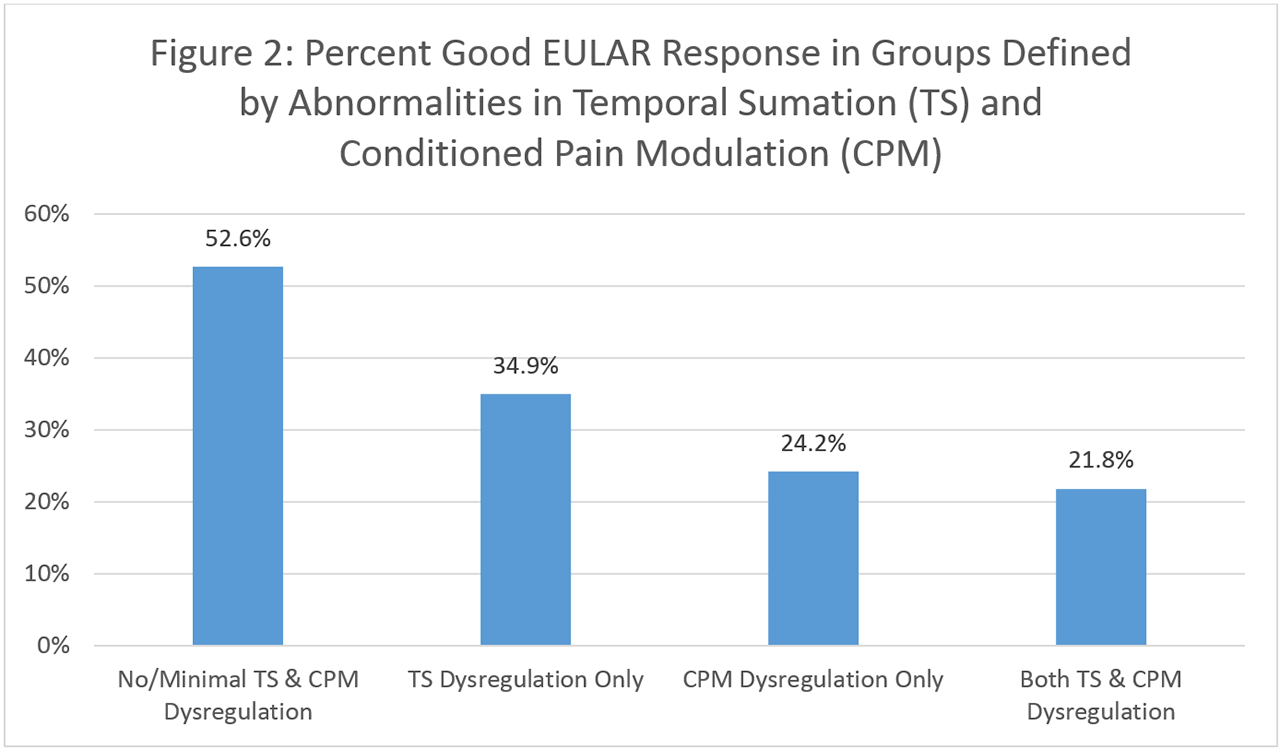
Results: Mean age of the population was 55.2 years. 83% of patients were female, and 70.3% seropositive. Mean baseline Disease Activity Score in 28 joints (DAS28-CRP) was 4.3. Patients with greater central dysregulation had lower percentages of good EULAR response (PPT: 24.6% vs. 36.7%, TS: 26.3% vs. 34.6%, CPM: 22.5% vs. 40.3%) (Figure 1) and lower adjusted ORs of good EULAR response (PPTs: OR 0.59 (95% CI 0.28-1.23), TS: OR 0.60 (95% CI 0.27-1.34), CPM: OR 0.40 (95% CI 0.19-0.83)) than those with least dysregulation (Table 1). However, only the OR for CPM reached statistical significance. Percent good EULAR response decreased with increasing number of abnormalities in pain centralization mechanisms (neither TS and CPM: 52.6%, only TS dysregulation: 30.8%, only CPM dysregulation: 24.4%, both TS and CPM dysregulation: 22.1%) (Figure 2). The adjusted OR for good EULAR response was 0.23 (95% CI 0.07-0.73) for patients with both TS and CPM dysregulation compared to those without TS and CPM dysregulation (Table 1).
Conclusion: In this study, high pain centralization, particularly impaired pain inhibition, was associated with poor DMARD response. Physicians should consider pain centralization as a possible reason why some patients fail to reach low disease activity or remission, despite treatment with DMARDs. Such patients may benefit from adjunctive therapy (e.g. serotonin norepinephrine reuptake inhibitors), rather than escalation of DMARD therapy.
To cite this abstract in AMA style:
Heisler A, Song J, Dunlop D, Wohlfahrt A, Bolster M, Marder W, Bingham C, Clauw D, Neogi T, Lee Y. Association of Pain Centralization with DMARD Response in Active RA [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/association-of-pain-centralization-with-dmard-response-in-active-ra/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-pain-centralization-with-dmard-response-in-active-ra/