Session Information
Date: Monday, November 13, 2023
Title: (1345–1364) Reproductive Issues in Rheumatic Disorders Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Whether the timing of menstruation impacts disease activity or severity among women with SLE or RA is poorly understood. We evaluated systemic rheumatic disease (SRD) flares related to the timing of menses, along with demographic, medical, and lifestyle characteristics among pre-menopausal women with self-reported diagnoses of SLE or RA.
Methods: We enrolled women ages 18-65 evaluated by a Hospital for Special Surgery rheumatologist ≥2 times from 2020-2022 in the Rheumatology Women’s Reproductive Health and Wellness Cohort. This analysis includes participants who self-reported SLE or RA diagnoses and provided information on SRD flares and menstrual cycles. We conducted descriptive analyses to compare self-reported demographics, lifestyle factors, medication use, and SRD flare activity overall and related to timing of menstrual cycles, between women with self-reported RA and SLE. We excluded women self-reporting overlapping SLE and RA diagnoses, though participants may have additional SRD diagnoses.
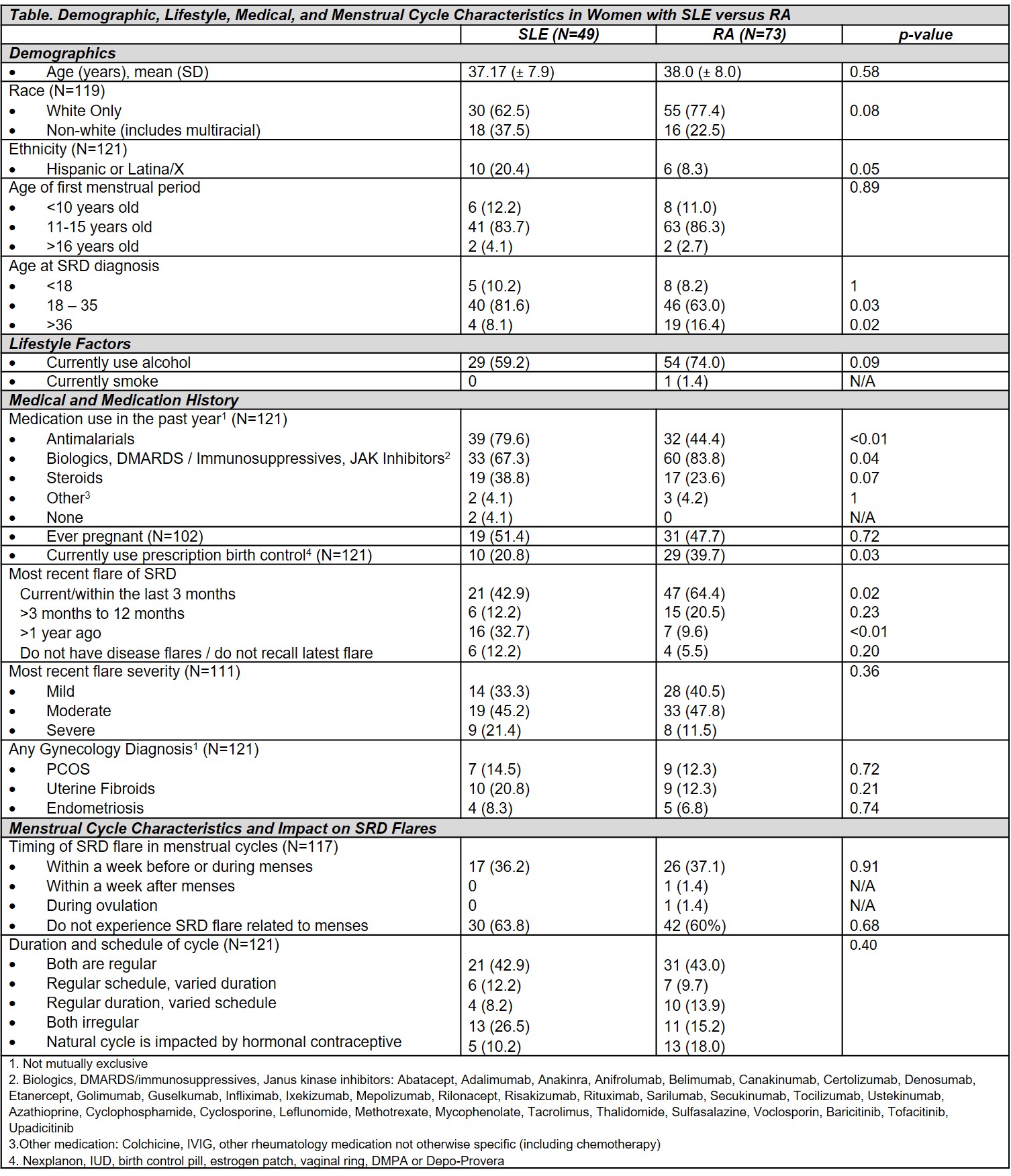
Results: Out of 812 cohort participants,307 (37.8%) pre-menopausal women responded to our questions on menstruation. The current analysis includes 122 of the respondents (40%) who self-reported an SRD diagnosis of SLE (N=49) or RA (N=73). 85 (71.4%) participants were White, 16 (13.2%) were Hispanic or Latina/Latinx, and mean age was 37.6 years. Of those who reported medication use, women with RA were more likely to use biologics, DMARDS/immunosuppressives, or Janus kinase inhibitors within the last year (83.8% RA vs. 67.3% SLE, p< 0.01), while those with SLE more commonly used antimalarials (79.6% SLE vs. 43.8% RA p< 0.01). Fewer women with SLE used prescription birth control (20.8% vs. 39.7%, p=0.03). RA patients were also more likely to report a recent SRD flare within the last 3 months (64.4% vs. 42.9% p=0.02); however, SRD flares were most common in this time frame for both groups with comparable flare severity (mild, moderate, severe) between groups (Table). Of those answering our question on timing of SRD flare in their menstrual cycle, 39.1% reported any association of menstrual cycle timing with an SRD flare. Variation in the duration and schedule of menstrual cycles and the impact of participants menstrual cycles on SRD flares was consistent between SLE and RA groups. While the majority of participants in each group reported not experiencing SRD flares related to their menses, those who did typically experienced flares within one week before/during their menses (Table).
Conclusion: Our findings suggest that over a third of women with SLE or RA experience disease flares related to timing of menstruation, with most occurring before/during their menses. Our results highlight an important trend reported by many patients that may inform physician counseling and encourage closer monitoring during vulnerable phases of the menstrual cycle, allowing for timely intervention and better disease control. As cohort recruitment is ongoing, planned multivariable analyses adjusting for demographic, lifestyle, and medical conditions will investigate factors influencing this potential association.
To cite this abstract in AMA style:
Masto L, Smole A, Siegel C, Lieber S, Adurty S, Levine J, Stamm B, Mandl L, Lockshin M, Sammaritano L, Barbhaiya M. Association of Menstrual Cycles and Disease Flare Activity in Women with Systemic Lupus Erythematosus and Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/association-of-menstrual-cycles-and-disease-flare-activity-in-women-with-systemic-lupus-erythematosus-and-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-menstrual-cycles-and-disease-flare-activity-in-women-with-systemic-lupus-erythematosus-and-rheumatoid-arthritis/