Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The relationship between menopause and systemic rheumatic disease (SRD) severity in women with SRDs is poorly understood. Few studies evaluating this association suggest worsening disease activity in RA but improved disease activity in SLE (Shah et al. Cureus, 2020); however, to our knowledge, no study directly compares SRDs. We explored the association of menopause and self-reported disease activity in women with SRDs, comparing self-reported outcomes between women with RA and SLE specifically.
Methods: We enrolled women ages 18-65 evaluated by a Hospital for Special Surgery rheumatologist ≥2 times from 2020-2022 in the Rheumatology Women’s Reproductive Health and Wellness Cohort. This analysis includes women with an SRD confirmed by ICD-10 code-based algorithms who self-reported peri-menopause or menopause and completed demographic, medical history, and menopause questionnaires. We used descriptive statistics to compare patient-reported demographics, menopause symptoms, and SRD-related measures in SLE versus RA. In secondary analyses, we stratified the cohort by those reporting worsened SRD during/after menopause vs. those who did not.
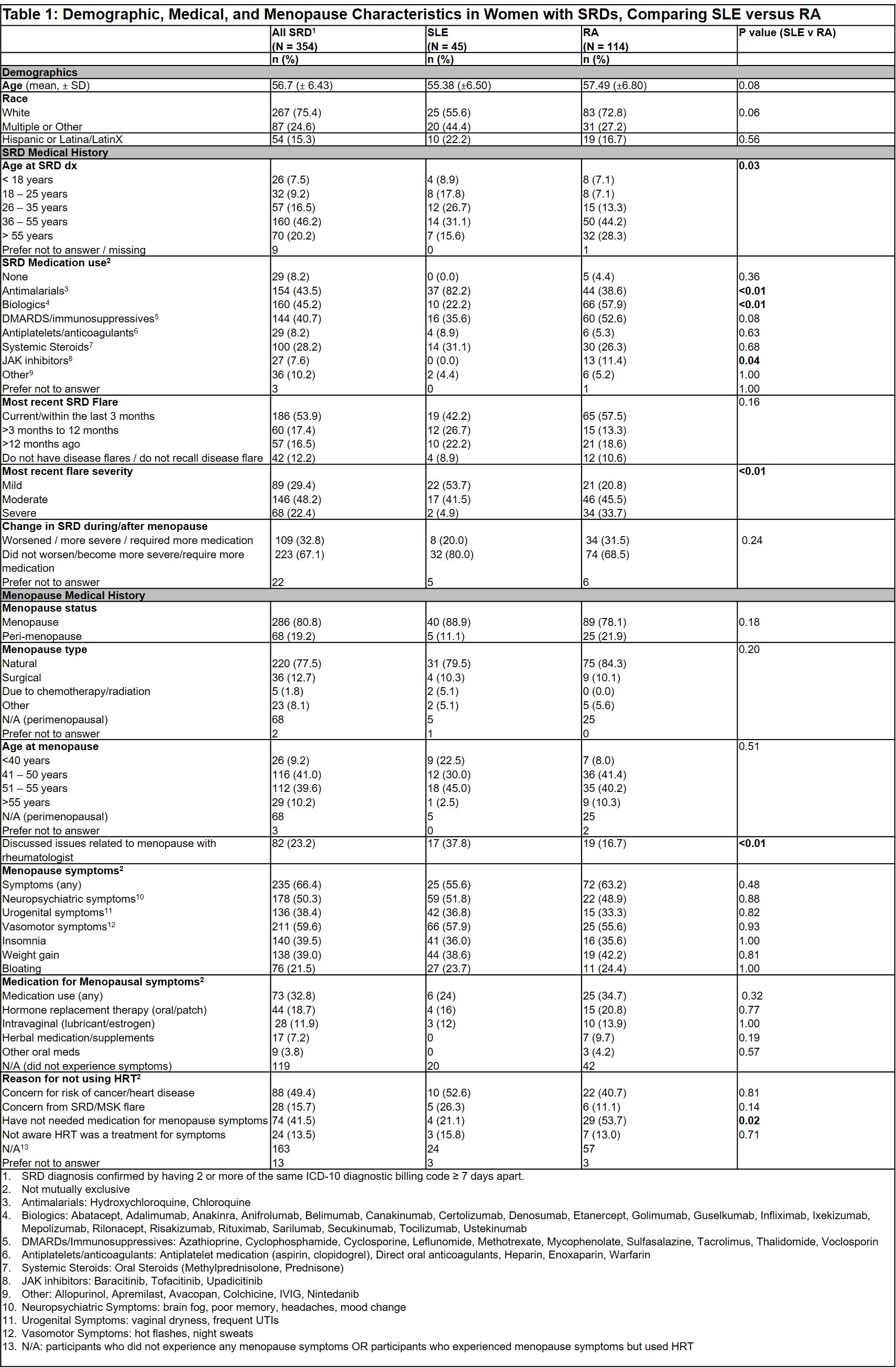
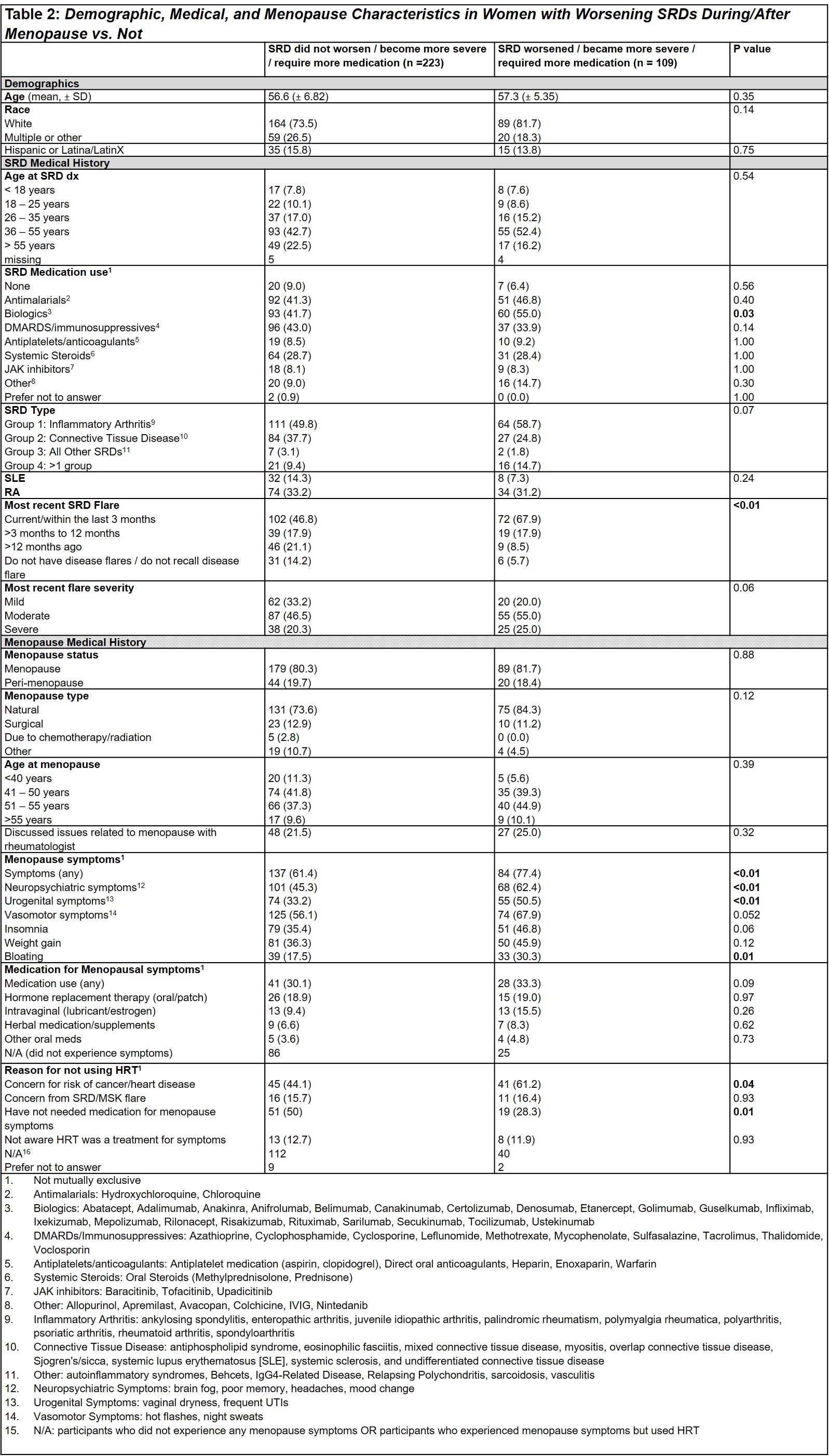
Results: Of 1,108 cohort participants, 354 (32%) had an SRD and self-reported menopause or peri-menopause (mean age: 56.7 ± 6.4 years, 267 [75.4%] White, 54 [15.3%] Hispanic or Latina/LatinX). 109 (32.8%) women with SRDs reported that their SRD “worsened/required more medication/was more severe” when asked how their condition changed during menopause, though this did not differ between women with SLE vs. RA (p=0.24). However, in RA vs. SLE, a higher proportion of peri-menopausal and menopausal women reported that their most recent SRD flare was “severe” (p< 0.01). Menopause symptoms and medication use for symptoms did not differ significantly between women with RA vs. SLE, yet women with SLE more commonly discussed issues related to menopause with their rheumatologist (37.8% vs. 16.7%, p< 0.01; Table 1). When stratified by self-report of SRD worsening during/after menopause versus not, SRD diagnosis did not differ. Women with worsening SRD reported more menopausal symptoms (84 [77.4%] vs.137 [61.4%], p< 0.01) with higher reports of neuropsychiatric symptoms (p< 0.01), urogenital symptoms (p< 0.01), and bloating (p< 0.05). They also more commonly used biologics (p=0.03), reported having a more recent SRD flare (p< 0.01), and cited concern for risk of cancer/heart disease as a reason for not using hormone replacement therapies to treat menopausal symptoms (p=0.04; Table 2).
Conclusion: Nearly a third of women with SRDs in our cohort report worsening disease associated with menopause, with this same group reporting more recent SRD flares and more menopausal symptoms. Although the association of menopause and SRD activity in SLE and RA was similar in our cohort, patients with SLE were over twice as likely to discuss menopausal issues with their rheumatologists than those with RA. Future multivariable analyses confirming these findings will help inform tailored clinical management of menopausal women with SRDs. Enhanced attention to and discussion of SRD flares and menopausal symptoms in women with SRDs may help contribute to optimizing mental and physical health.
To cite this abstract in AMA style:
Masto L, Smole A, Lan R, Parides M, Siegel C, Lieber S, Levine J, Stamm B, Mandl L, Lockshin M, Sammaritano L, Barbhaiya M. Association of Menopause and Systemic Rheumatic Disease Severity in Peri-Menopausal and Menopausal Women with Systemic Rheumatic Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-menopause-and-systemic-rheumatic-disease-severity-in-peri-menopausal-and-menopausal-women-with-systemic-rheumatic-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-menopause-and-systemic-rheumatic-disease-severity-in-peri-menopausal-and-menopausal-women-with-systemic-rheumatic-disease/