Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Total joint replacement (TJR) is the standard surgical treatment for end-stage hip and knee osteoarthritis (OA). Patient optimization may limit the need for early revision surgeries. Low bone mineral density (BMD) may cause periprosthetic fractures, osteolysis and implant migrations which can affect postoperative outcomes, but the data is limited. There is also no standardized approach to assess bone health prior to TJR. Our primary objective was to study the prevalence of low bone mass and its relationship to early revision arthroplasty.
Methods: We performed a retrospective, case-control, single-center study using Reading Hospital Joint Database. We reviewed charts of postmenopausal women who underwent hip and knee arthroplasty from January, 2013 to December, 2019 and identified patients who underwent early (within 5 years) revision arthroplasty for aseptic indications (“cases”). We matched each of the cases to 2 postmenopausal women who did not undergo a revision surgery during the time period (“controls”), matched for age at index surgery (+/- 5 years), timing of initial TJR (+/- 6 months) and type of TJR. We identified patients with BMD testing with DEXA (dual-energy X-ray absorptiometry) within 2 years of the index TJR. We collected data on patient characteristics including age, body mass index (BMI), use of vitamin D and calcium, chronic glucocorticoid (prednisone equivalent of 5 mg/day for > 3 months) and anti-osteoporotic therapy use. Late revision surgeries and infectious indications were excluded.
Results: We identified 25 postmenopausal women with elective TJR for OA who underwent early revision hip (n=11) and knee replacement (n=14) for aseptic indications. The mean age for index TJR was 70 years. The average duration between index and revision surgery was 22 months (12 months for hip and 30 months for knee revision).
Each of the postmenopausal women who underwent early joint revision (n=25) were matched to 2 postmenopausal women who did not undergo early revision surgery (n=50) during the study period (Table 1). Forty percent patients in the early revision group had documentation of a screening DEXA compared to 60 % patients in the non-revision group. Among patients who had DEXA, 7/10 (70%) had low bone mass (osteopenia or osteoporosis) in the early revision group compared to 17/31 (55%) in the non-revision group. Of the 4 patients with a history of fragility fracture in the early revision group, 75% underwent revision surgery within the first 2 months of index TJR (two due to periprosthetic fracture and one due to femoral loosening). The use of calcium and vitamin D was identified in 40% and 52% in the early revision group compared to 44% and 68%, respectively, in the non-revision group.
Conclusion: Our study found a lower rate of DEXA screening and a higher prevalence of low bone mass in the early revision group, which may suggest a higher prosthetic failure in patients with low bone mass. We were unable to assess the role of anti-osteoporosis medication on the outcome due to the small sample size. Further studies are needed to explore the impact of osteoporosis and its treatment on postoperative outcomes, particularly in those with a history of a prior fragility fracture.
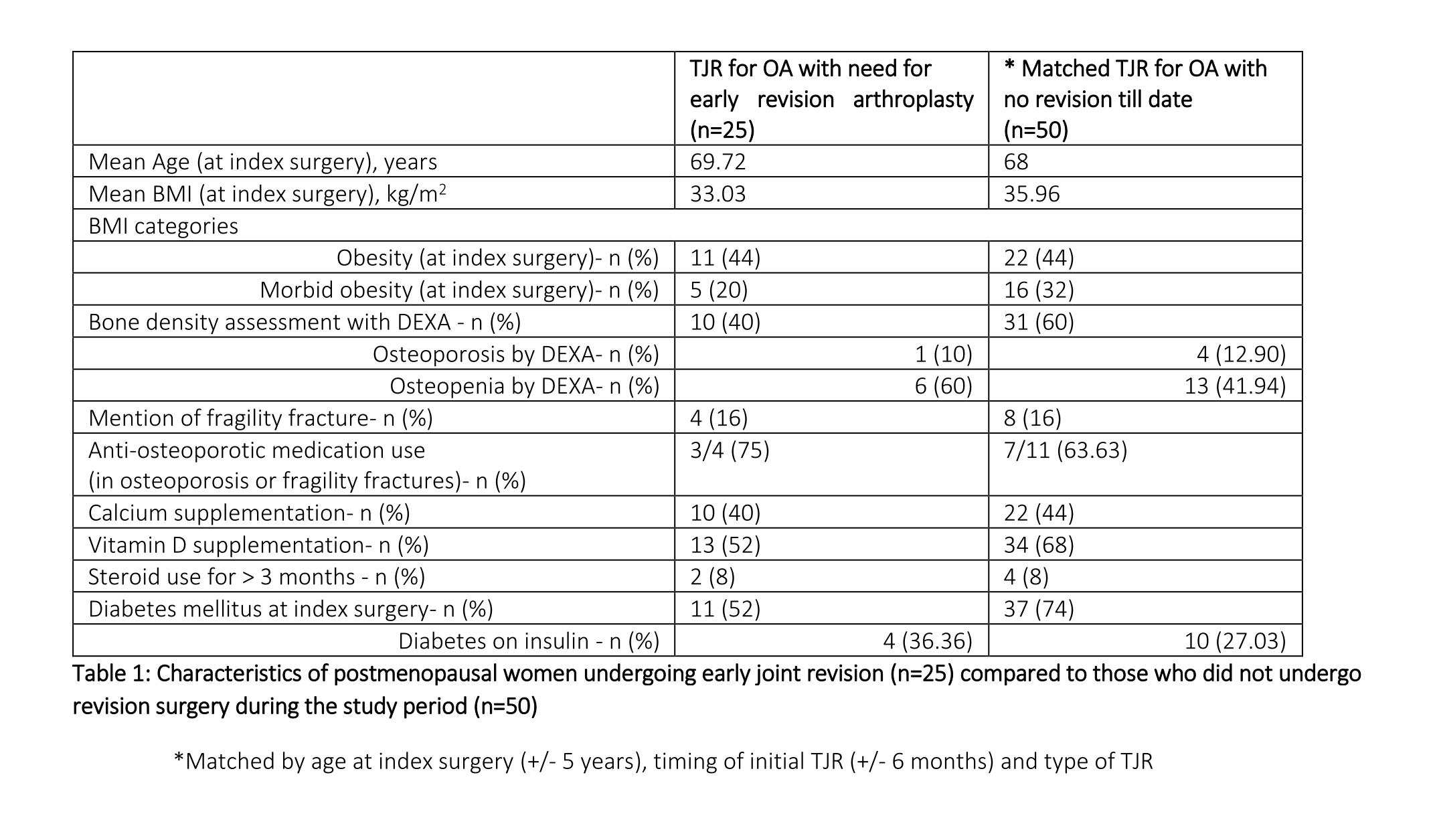 Table 1: Characteristics of postmenopausal women undergoing early joint revision (n=25) compared to those who did not undergo revision surgery during the study period (n=50) *Matched by age at index surgery (+/- 5 years), timing of initial TJR (+/- 6 months) and type of TJR
Table 1: Characteristics of postmenopausal women undergoing early joint revision (n=25) compared to those who did not undergo revision surgery during the study period (n=50) *Matched by age at index surgery (+/- 5 years), timing of initial TJR (+/- 6 months) and type of TJR
To cite this abstract in AMA style:
Dhital R, Nicholas P, Emkey G, Donato A. Association of Low Bone Density with Need for Early Revision After Elective Joint Replacement for Osteoarthritis in Postmenopausal Women [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/association-of-low-bone-density-with-need-for-early-revision-after-elective-joint-replacement-for-osteoarthritis-in-postmenopausal-women/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-low-bone-density-with-need-for-early-revision-after-elective-joint-replacement-for-osteoarthritis-in-postmenopausal-women/
