Session Information
Date: Sunday, November 8, 2020
Title: Patient Outcomes, Preferences, & Attitudes Poster II: Miscellaneous Rheumatic Diseases
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Over 33 percent of American adults have low health literacy, which limits their ability to understand basic health information and make healthcare decisions. A component of health literacy is health numeracy (quantitative skills). Low health literacy has been associated with negative psychological and patient reported outcomes in other disease states including lower self-efficacy, reduced quality of life, and higher rates of depression. However, the relationship between health literacy and psychological outcomes has not been evaluated in SLE. The objective of this study was to assess the relationship of health literacy with psychological and patient-reported outcomes in SLE.
Methods: SLE patients meeting SLICC criteria were recruited from an academic university clinic from March 2019 through January 2020. Self-reported health literacy and numeracy were assessed using the Basic Health Literacy Screen (BHLS) and the 3-item Subjective Numeracy Scale (SNS-3). Low health literacy was defined as BHLS < 12 and low numeracy as SNS3 ≤ 14. Patients completed assessments for depression (Patient Health Questionnaire, PHQ9), fibromyalgia severity score (FSS), and self-reported cognitive dysfunction. Additionally, PROMIS Short-Forms for General Self-Efficacy and for Managing Treatments and Medications were obtained. We evaluated relationships between health literacy, self-efficacy and psychological covariates using descriptive statistics. Fisher’s exact testing was performed for categorical measures and two-sample t-tests were performed for continuous measures.
Results: The study included 172 patients with SLE with average age 41 years, 94% female, and 61% African American. Mean clinical SLEDAI was 3.17. We found 14% of patients had low health literacy, while 45% of patients had low numeracy.
Health Literacy:
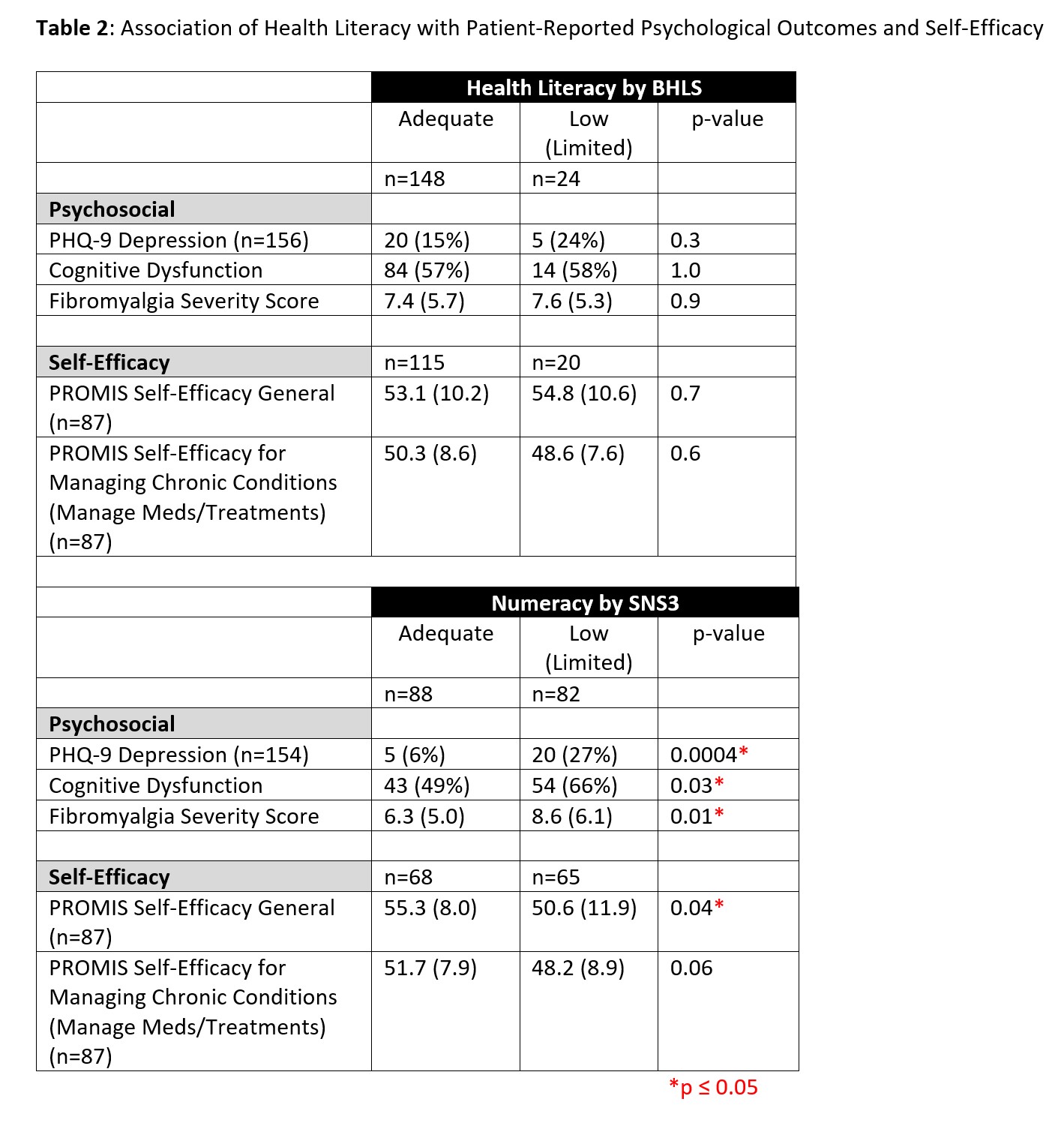
There were no differences in demographics or patient-reported outcomes between patients with low versus adequate health literacy (Tables 1-2).
Numeracy:
Patients with lower numeracy were more likely to be African American, less likely to be a college graduate, more likely to have income < $50,000 annually, and more likely to be on Medicaid insurance or disability (Table 1). Those with lower numeracy were more likely to have depression, higher fibromyalgia severity scores, and cognitive dysfunction (Table 2). Additionally, patients with lower numeracy had worse self-efficacy by PROMIS Self-Efficacy (50.6 vs 55.3, p=0.04).
Conclusion: Lower numeracy was associated with higher rates of depression, higher fibromyalgia severity, lower self-efficacy and lower socioeconomic status factors. This data suggests numeracy may be an important factor to consider in patient counseling, particularly patients with concomitant depression or other psychiatric comorbidities. Future studies should evaluate the role of health literacy with other lupus outcomes.
To cite this abstract in AMA style:
Maheswaranathan M, Rogers J, Eudy A, Sun K, Bailey S, Hastings S, Clowse M. Association of Health Literacy and Numeracy with Patient Reported Psychological Outcomes [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/association-of-health-literacy-and-numeracy-with-patient-reported-psychological-outcomes/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-health-literacy-and-numeracy-with-patient-reported-psychological-outcomes/