Session Information
Date: Sunday, November 7, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Manifestations (0855–0896)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: HCQ levels reflect adherence and have been shown to correlate with SLE outcomes. However, HCQ levels have not been studied in the context of a novel conceptual model which categorizes SLE activity into Type 1 (including arthritis, rash, nephritis) and Type 2 manifestations (including myalgias, mood disturbance, and cognitive dysfunction). We hypothesized that HCQ levels would inversely correlate with Type 1 but not Type 2 SLE activity.
Methods: Those meeting ACR or SLICC classification criteria for SLE were recruited from an academic lupus clinic. We measured whole blood HCQ levels using liquid chromatography coupled to mass spectrometry. Patients were categorized by HCQ levels as under-exposed (HCQ < 200 ng/ml), subtherapeutic (HCQ between 200-1000 ng/ml), or therapeutic (HCQ >1000 ng/ml). Type 1 SLE activity measures included Type 1 Physician Global Assessment (PGA) and SLEDAI. Type 2 SLE activity measures included Type 2 PGA, patient-reported Polysymptomatic Distress (PSD) score, and depression based on the Patient Health Questionnaire-2. SLE groups were defined as Minimal (low Type 1 and 2 activity), Type 1 (high Type 1 and low Type 2 activity), Mixed (high Type 1 and 2 activity), and Type 2 (low Type 1 and high Type 2 activity). Self-reported adherence was measured using the visual analog scale of the Medication Adherence Self-Report Inventory. We used the Chi-squared and Kruskal-Wallis tests to examine differences across patient groups.
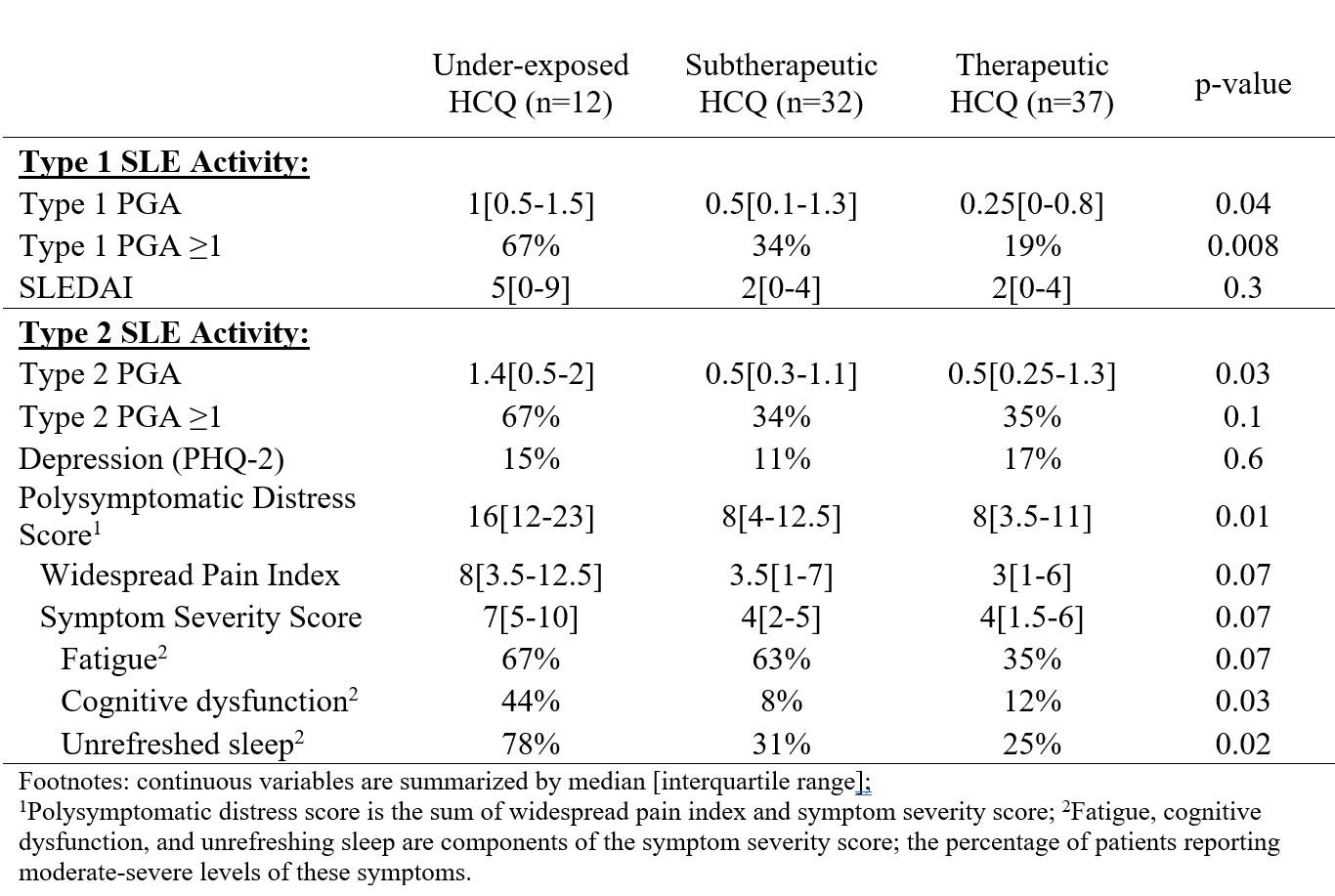
Results: This analysis included 81 patients (median age 42, 90% female, 73% Black, 51% < college education, 39% married or cohabiting, 29% with annual household income >$50,000, and 58% with private insurance). HCQ levels were under-exposed in 15%, subtherapeutic in 39%, and therapeutic in 46% of patients (Table 1).
Patients with therapeutic HCQ levels were more likely to have private insurance and a trend for older age and higher income. Self-reported adherence was similarly high among the three HCQ groups. Patients with lower HCQ levels are more likely to have lower creatinine, but weight and HCQ dose prescribed did not appear to play a consistent role in therapeutic drug level.
Lower HCQ levels were significantly associated with both higher Type 1 and Type 2 SLE activity. Patients with lower HCQ levels self-reported a higher PSD score, more cognitive dysfunction and nonrestorative sleep. There was also a trend for patients with lower HCQ blood levels to have more fatigue, areas of pain, and higher symptom severity scores (Table 2).
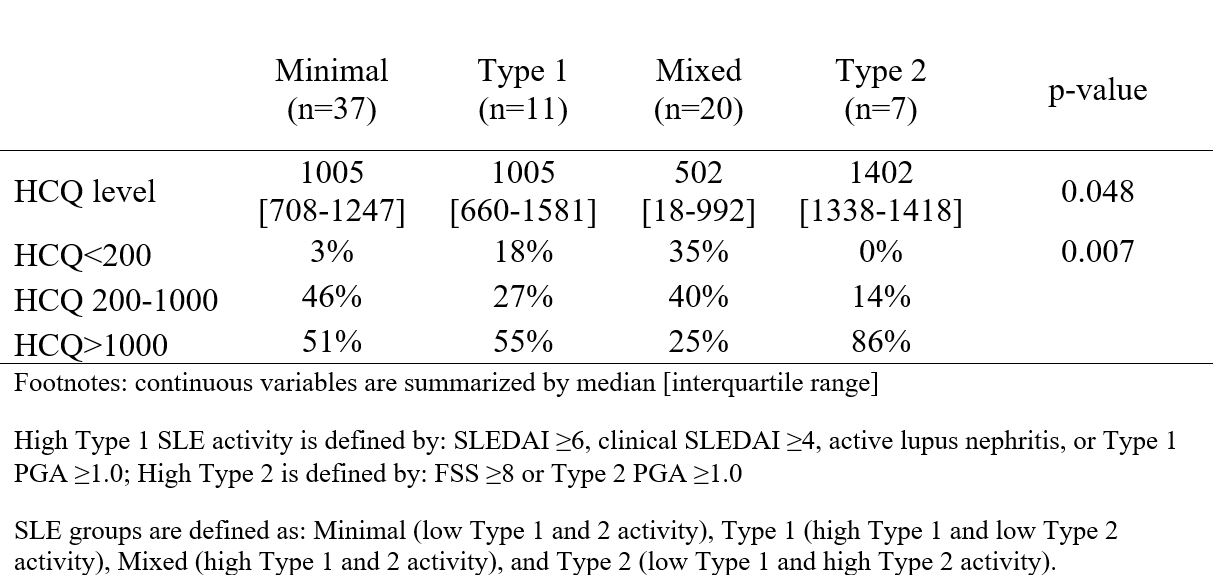
Comparing HCQ levels across SLE groups, patients with Mixed SLE activity had significantly lower HCQ levels compared to all other patients (Table 3).
Conclusion: More than half of the patients had lower than therapeutic HCQ blood levels, and surprisingly, this was associated with both higher Type 1 and Type 2 SLE activity. Although Type 2 SLE manifestations are conventionally thought to be noninflammatory, their inverse association with HCQ blood levels in patients with concurrent Type 1 SLE activity suggest that in some SLE patients, immunologic activity may contribute to these debilitating symptoms.
To cite this abstract in AMA style:
Sun K, Eudy A, Rogers J, Criscione-Schreiber L, Sadun R, Doss J, Brady K, Alexander R, Conklin J, Bloch R, Clowse M. Association of HCQ Blood Levels with Type 1 and 2 SLE Activity [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-of-hcq-blood-levels-with-type-1-and-2-sle-activity/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-hcq-blood-levels-with-type-1-and-2-sle-activity/