Session Information
Date: Sunday, October 26, 2025
Title: (0357–0386) Patient Outcomes, Preferences, & Attitudes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Glucocorticoids (GCs) are used long-term by approximately 1% of the adult population and contribute to excess morbidity and mortality. We prospectively assessed Glucocorticoid Toxicity Index (GTI) scores at 6 months in a real-world cohort of individuals using GCs in rheumatology clinic given the limited published real-world data involving GTI scores.
Methods: We developed a prospective cohort of adult patients with rheumatic diseases in a large academic hospital and prospectively assessed GC toxicity as measured by the GTI, patient-reported quality-of-life (including the 36-Item Short Form Survey [SF-36] scale and component scores, and EQ5D-visual analogue scale [VAS]), and physician clinic visits. Data on healthcare utilization are obtained by manual medical record review. We evaluated overall GTI (Cumulative Worsening Score [CWS], a measure of any toxicity, and Aggregate Improvement Scores [AIS], which assess both worsening [increasing scores] and improvement [decreasing scores]) and individual domains at 6 months. We evaluated the relationship of 6-month GTI scores to cumulative GC exposure, quality-of-life measures, and clinic visits using unadjusted and multivariable (adjusted for age, sex, and disease activity) Pearson correlation coefficients (rho).
Results: We evaluated the first 90 patients enrolled (mean age 60 years, 62% female, 90% White, 41% with PMR and/or GCA) and the first 74 who completed 6-month follow-up (Table 1). The majority of patients (81%) had active disease at enrollment. The mean (SD) current GC dose was 33.4 (19.1) prednisone-equivalent mg, and most were also receiving a DMARD (65, 72%). Over the 6-month follow-up period, the median (IQR) cumulative GC exposure was 2114 (1185, 3080) prednisone-equivalent mg, or approximately 11.6 mg/day. The median (IQR) overall 6-month GTI CWS was 44 (20, 93) and GTI AIS was 3 (-42, 54). The most common GTI domain in which individuals experienced worsening was the Neuropsychiatric domain, followed by the Body Mass Index, Blood Pressure, and Skin domains (Figure). The unadjusted correlation coefficient between GTI CWS scores and 6-month GC exposure was 0.28 (95% CI: 0.06-0.48); this was diminished in the adjusted analysis (Table 2). Higher GTI CWS was associated with numerically lower (i.e., worse) SF-36 scale and component scores. There was a weak positive association between the GTI CWS and the number of clinic visits though this was not statically significant.
Conclusion: In this real-world prospective cohort of individuals with autoimmune diseases receiving GCs, most people experienced various GC toxicities over 6 months with a predominant proportion with neuropsychiatric toxicities. Improvement in some GC toxicities was also observed, as evidenced by the markedly lower 6-month AIS value compared to the 6-month CWS value. Higher GTI CWS scores were numerically associated with worse quality-of-life. Presence of any GC toxicities correlated more strongly with outcomes than net overall change in toxicity. As shown in other studies, the relationship between cumulative GC exposure and GC toxicity is imperfect, emphasizing the importance of measuring GC toxicity directly.
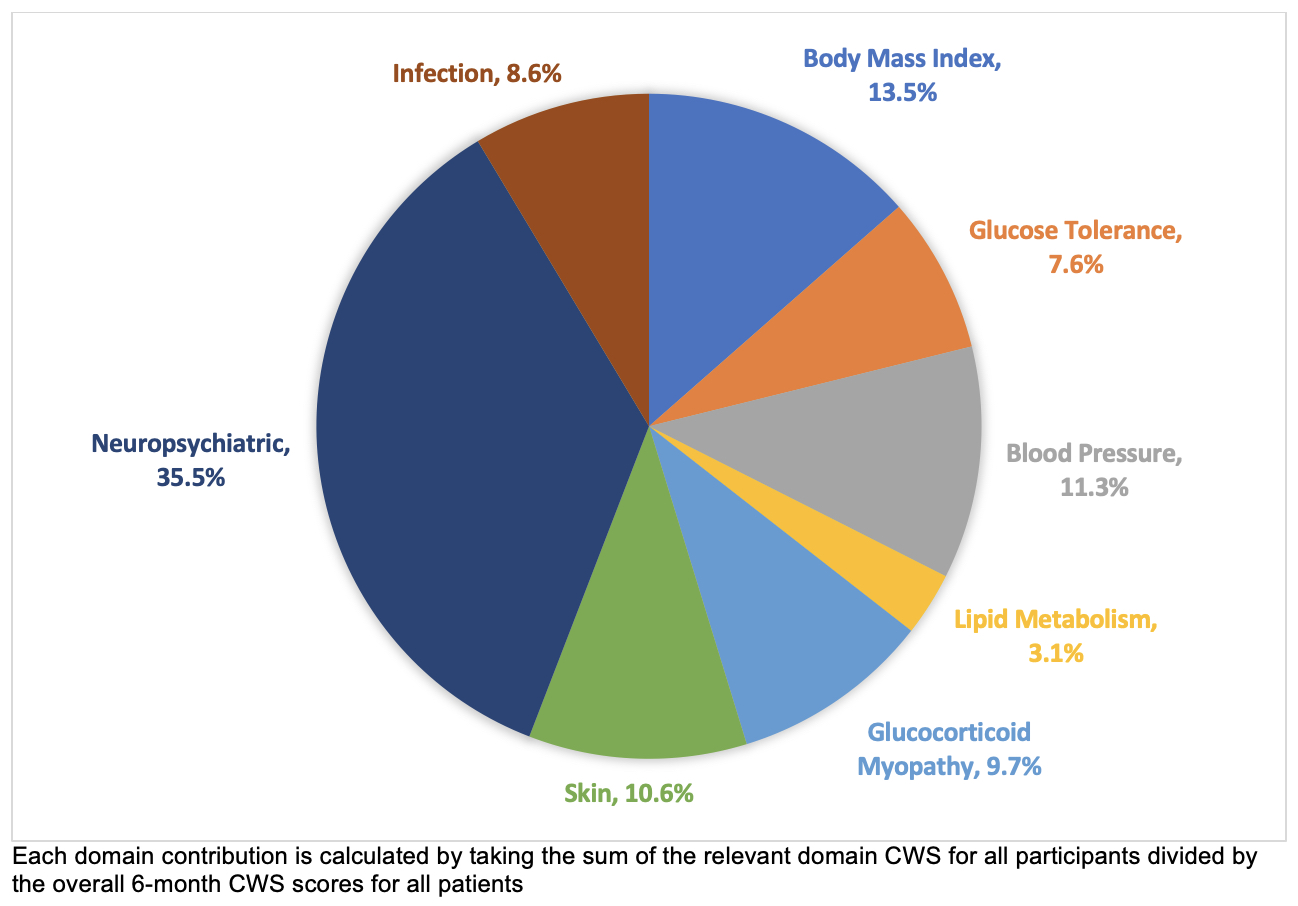 Table 1. Demographic, Disease, and Treatment Characteristics of Participants in LONG-TOX at Enrollment (Baseline) and 6 Months
Table 1. Demographic, Disease, and Treatment Characteristics of Participants in LONG-TOX at Enrollment (Baseline) and 6 Months
.jpg) Figure 1. Contribution of Glucocorticoid Toxicity Index (GTI) Domain Scores to Overall GTI Scores at 6 months
Figure 1. Contribution of Glucocorticoid Toxicity Index (GTI) Domain Scores to Overall GTI Scores at 6 months
.jpg) Table 2. Association of 6-month Glucocorticoid Toxicity Index Cumulative Worsening Scores with Quality-of-Life, Cumulative Glucocorticoid Exposure, and Healthcare Resource Utilization
Table 2. Association of 6-month Glucocorticoid Toxicity Index Cumulative Worsening Scores with Quality-of-Life, Cumulative Glucocorticoid Exposure, and Healthcare Resource Utilization
To cite this abstract in AMA style:
Patel N, Wang J, Jha I, McMahon G, Chiha T, Choi H, Stone J. Association of Glucocorticoid Toxicity Index Scores with Quality-of-Life and Healthcare Resource Utilization at 6 Months in a Real-World Cohort of Individuals Receiving Glucocorticoids [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-of-glucocorticoid-toxicity-index-scores-with-quality-of-life-and-healthcare-resource-utilization-at-6-months-in-a-real-world-cohort-of-individuals-receiving-glucocorticoids/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-glucocorticoid-toxicity-index-scores-with-quality-of-life-and-healthcare-resource-utilization-at-6-months-in-a-real-world-cohort-of-individuals-receiving-glucocorticoids/
