Session Information
Date: Monday, October 27, 2025
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Sjögren’s Syndrome (SS) is a multisystemic autoimmune disease that causes hypofunction of salivary and lacrimal glands, manifesting in xerostomia and xerophthalmia among other systemic manifestations. Unstimulated whole salivary flow rate (UWSF) is a test used to quantify saliva production, a decrease in USWF rate impacts the quality of life in patients with SS. Similarly, dry eye tests are useful tools in everyday clinical practice to identify inflammatory damage to the ocular surface. An abnormal UWSF, along with positive serology, a reduced Schirmer’s test, and a positive minor salivary gland biopsy is included in the 2016 ACR/EULAR SS classification criteria. However, the association between UWSF and dry eye tests is poorly known. We aimed to explore if there is an association between UWSF and dry eye severity.
Methods: A cohort of rheumatic patients with dry eye disease (DED) (2015-2024) was analyzed. Patients aged 18-years or older, with DED symptoms and primary SS diagnosis (according to ACR-EULAR 2016 criteria) were included. Patients were divided into two groups according to UWSF in 5 minutes (group 1: UWSF ≤0.5 ml/5min, group 2: UWSF >0.5 ml/5min). MSG biopsy, tear film osmolarity (OSM), matrix metalloproteinase 9 (MMP-9), Ocular Surface Disease Index (OSDI), Tear break-up time (TBUT), SICCA Ocular Surface Staining (SICCA OSS), and Schirmer tear test with and without anesthesia (STT) were evaluated. Only the worst eye was included, which was selected as the eye with the higher SICCA OSS score. Associations and results were presented using (frequencies [%], mean ± SD, median [IQR]), and we used Chi2, Mann-Whitney U, or Student’s tests as appropriate. Institutional ethics committee approval was received; all participants provided written informed consent.
Results: Eighty-nine patients with primary SS were included, the mean age was 52.6 ± 12.8 years, and 97.7% (87/89) were women. Forty-three (48.3%) patients had a UWSF ≤0.5 ml/5 min, and 46 (51.7%) patients had a UWSF >0.5 ml/5 min. We observed a higher proportion of patients with positive MMP-9 in the UWSF ≤0.5 ml/5 min group (15/43,34.9%) than those with a UWSF >0.5 ml/5 min (7/46,15.2%; p=0.041). Patients with UWSF ≤0.5 ml/5 min also showed higher OSDI scores (48.85 ± 27.83) than patients with UWSF >0.5 ml/5 min (34.76 ± 21.58; p=0.010). There was no difference in SICCA OSS scores, Schirmer’s tear test with or without anesthesia, tear film osmolarity, and tear break-up time.
Conclusion: Patients with low salivary flow had greater ocular surface damage and more dry eye disease symptoms.
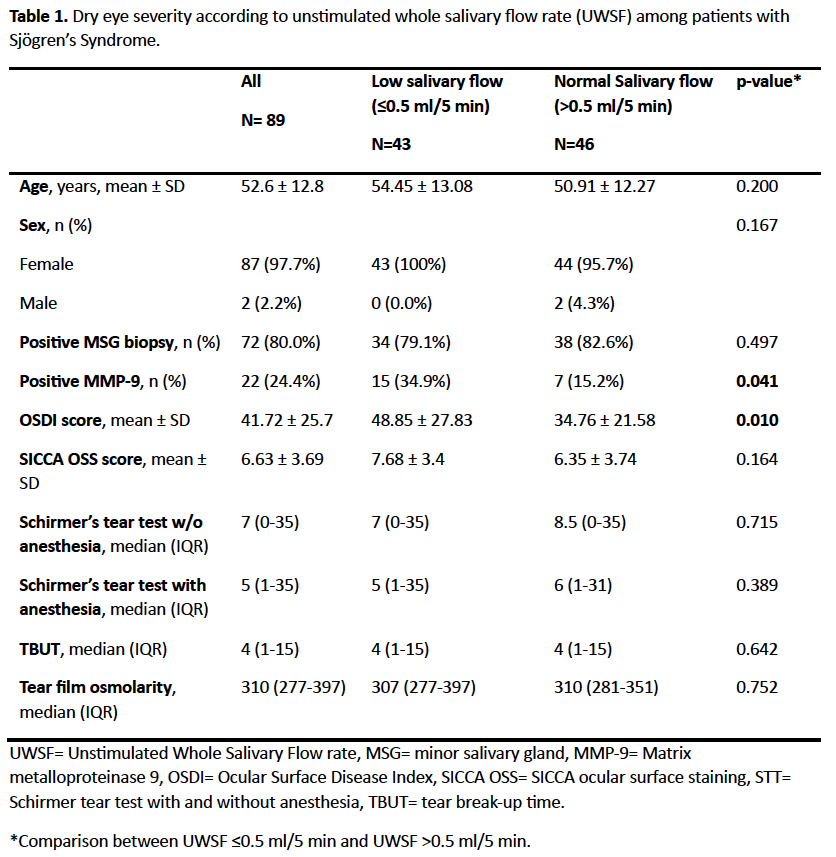 Table 1. Dry eye severity according to unstimulated whole salivary flow rate (UWSF) among patients with Sjögren’s Syndrome.
Table 1. Dry eye severity according to unstimulated whole salivary flow rate (UWSF) among patients with Sjögren’s Syndrome.
To cite this abstract in AMA style:
Riega-Torres J, Palomo-Arnaud K, Martinez-Delgado J, Morales-Wong F, Mohamed-Hamsho J, Mata-Riega V, Cantu-Zapata I, Medina-Gomez L, Betancourt-De la Torre M, Chong-Amezcua A, Galarza-Delgado D, Mohamed-Noriega K. Association Of Dry Eye Severity With Salivary Flow In Patients With Primary Sjögren’s Syndrome [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-of-dry-eye-severity-with-salivary-flow-in-patients-with-primary-sjogrens-syndrome/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-dry-eye-severity-with-salivary-flow-in-patients-with-primary-sjogrens-syndrome/
