Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Youth with childhood-onset systemic lupus erythematosus (cSLE) have increased risk of serious infection. It is unknown how much of this risk is due to inherent cSLE-related immune system dysfunction versus modifiable factors such as choice of immunosuppressant and glucocorticoid dosing. We aimed to compare hospitalized infection rates in youth with cSLE on different disease-modifying anti-rheumatic drugs (DMARDs).
Methods: We included youth ≤18 years with cSLE treated at two large pediatric rheumatology centers between 2009-2022. Clinical and demographic data were extracted from electronic health records and inpatient encounters in the Pediatric Health Information System (PHIS) dataset. Each child was classified by the first DMARD received after diagnosis. Hospitalized infections were defined by ICD-9 and ICD-10 codes and, for bacterial infections, by antibiotic use. Summary statistics were performed for youth with cSLE with and without lupus nephritis (LN) at time of first DMARD initiation. Frequency of hospitalization with infection was calculated over the first year of treatment in youth included in each DMARD group exposure group and stratified by LN status. Among those with LN at time of first DMARD initiation, the rate of infection in youth exposed to cyclophosphamide versus mycophenolate was compared using Cox proportional hazard regression, adjusting for concomitant rituximab exposure and oral corticosteroid dose; in those without LN, infection rates were compared between mycophenolate and azathioprine. Inverse probability of treatment weighting (IPTW) was used in all regression modeling to account for confounding by baseline DMARD indication.
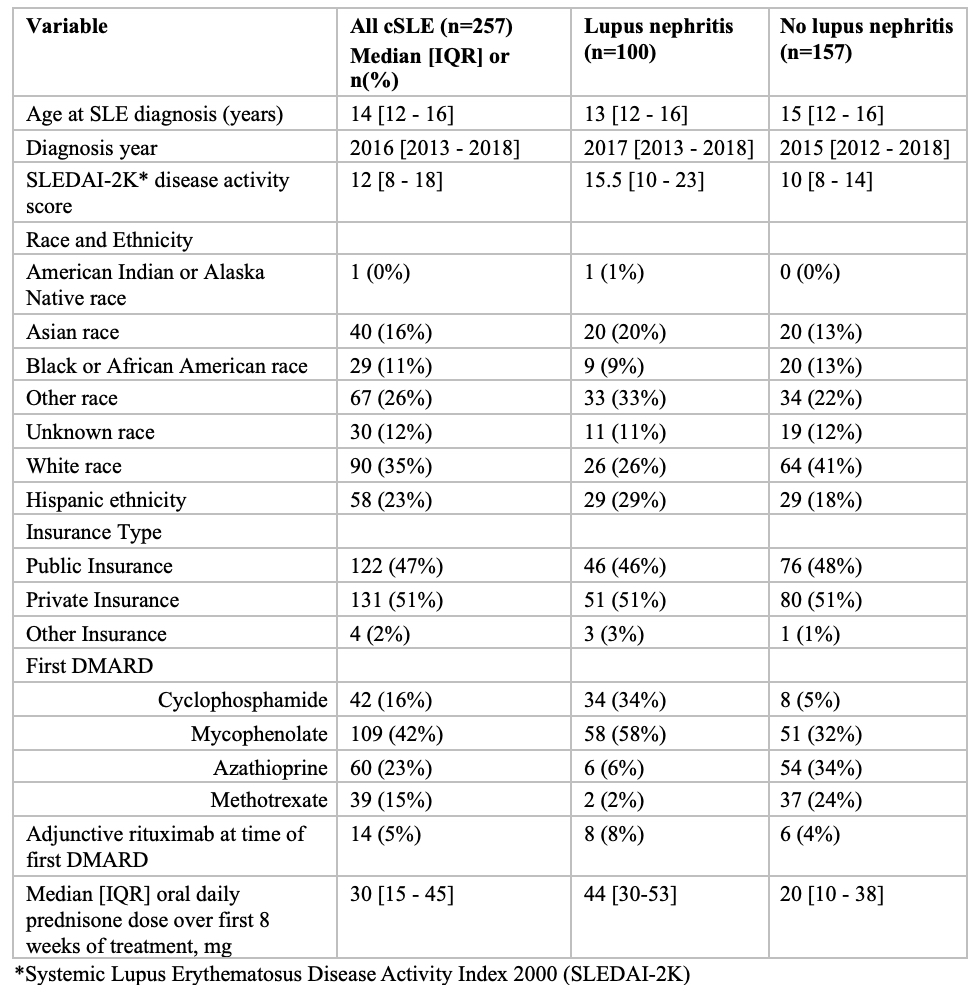
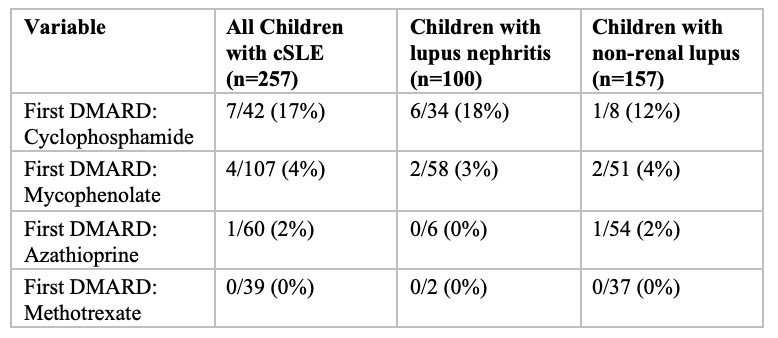
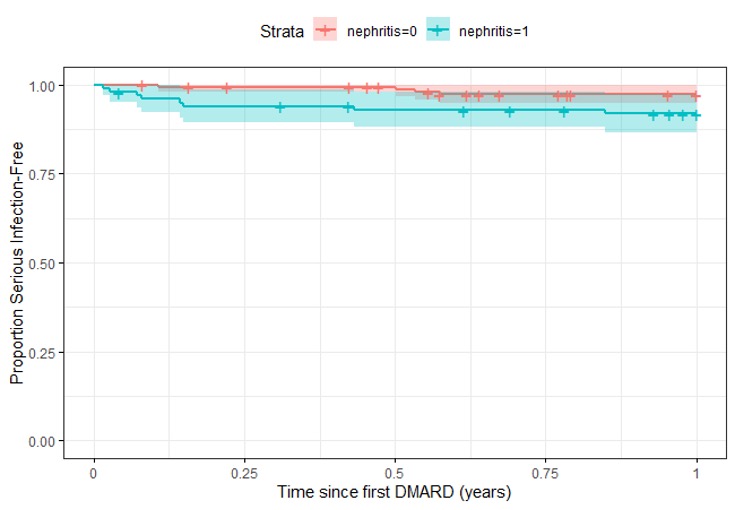
Results: We identified 257 youth with cSLE, of whom 100 (39%) had LN (Table 1). Of these, 12 (5%) had ≥1 hospitalization with infection within one year of DMARD initiation, including 8 (8%) youth with LN, and 4 (2.5%) of those without LN. Infections were numerically more common in youth with LN and occurred most frequently within 3 months of beginning treatment (Figure 1). The highest hospitalized infection rate (17%) was among children treated with cyclophosphamide (Table 2). In IPTW-adjusted models, children with LN treated with mycophenolate had lower risk of infection (HR 0.12; CI 0.019 – 0.88, p-value=0.036) compared to those treated with cyclophosphamide; oral corticosteroid dose was not significantly associated with infection. Among those without LN, mycophenolate did not differ from azathioprine in infection risk (HR 1.67, CI 0.56-4.99, p-value=0.4). Higher oral corticosteroid dosing (per 1mg/day, averaged over 8 week periods) was associated with a HR for infection of 1.10 (CI 1.05 – 1.15, p-value < 0.001).
Conclusion: We observed higher hospitalized infection rates in children with cSLE complicated by LN compared to those without nephritis. Among children with LN, those who received cyclophosphamide had more infections than those who received mycophenolate, which persisted after adjusting for baseline differences between groups and concomitant medications including oral corticosteroid dose. Higher oral corticosteroid doses were associated with increased hospitalized infection risk among those without LN.
To cite this abstract in AMA style:
Roberts J, Faino A, Brown M, Alonzi G, Bryan M, Burn C, Chang J, Cogen J, Naik N, Patel K, Zhang E, Son M, Morgan E. Association of Disease-Modifying Anti-Rheumatic Drug Selection with Hospitalized Infection in Youth with Childhood-Onset Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-disease-modifying-anti-rheumatic-drug-selection-with-hospitalized-infection-in-youth-with-childhood-onset-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-disease-modifying-anti-rheumatic-drug-selection-with-hospitalized-infection-in-youth-with-childhood-onset-systemic-lupus-erythematosus/