Session Information
Date: Sunday, November 17, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Ultrasound (US) is a valuable tool for enhancing disease activity assessment in psoriatic arthritis (PsA) by providing detailed visualization of both inflammatory and structural changes. Despite the established associations of various contextual factors with US abnormalities in PsA, the extent and significance of these associations remain unclear. Our study aims to investigate the impact of contextual factors on the presence and severity of sonographic lesions in patients with active PsA.
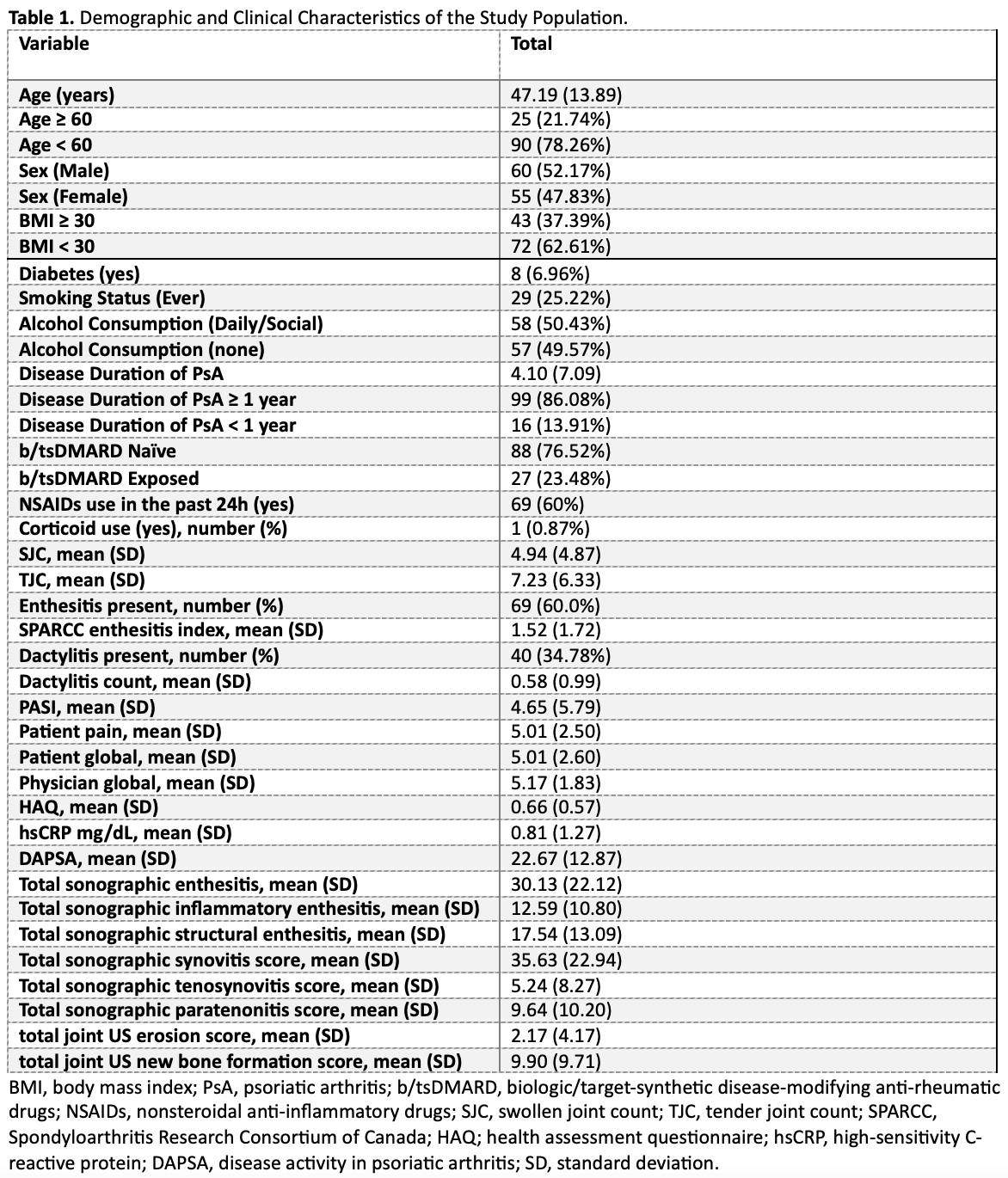
Methods: In a cross-sectional study, 115 patients with active PsA underwent a comprehensive US evaluation for inflammatory (inf) and structural (str) lesions like synovitis, enthesitis, peritenonitis (PTI), tenosynovitis (TN), bone erosion (BE), and new bone formation (NBF), with semi-quantitative B-mode and Doppler scores. The US protocol was extensive, covering 64 joints, 36 tendons, and 16 entheses. Total summary scores for each domain were analyzed using t-tests and linear multivariable regression by age (≥60, < 60), sex, body mass index (BMI) (≥30, < 30), diabetes, alcohol (any, none), smoking, disease duration (≥1, < 1 years), and biological/target-synthetic disease-modifying anti-rheumatic drug (b/tsDMARDs) exposure.
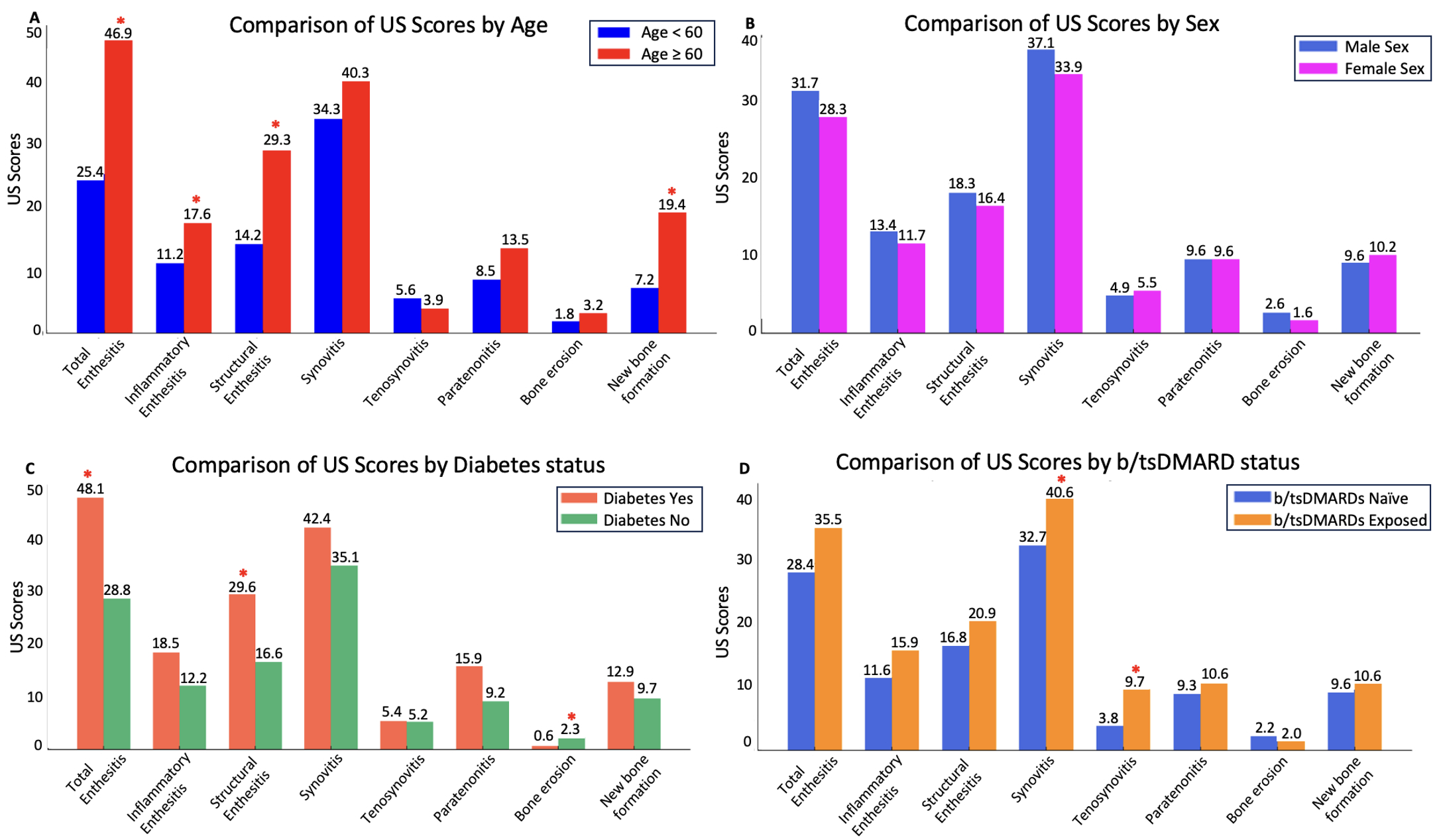
Results: Among the 115 patients studied (mean age 47.1 years, 47.8% females), the average Disease Activity in Psoriatic Arthritis (DAPSA) score was 22.6. The mean US scores were 35.6 for synovitis and 30.1 for total enthesitis. Detailed population characteristics are provided in Table 1. Key findings included significantly higher sonographic scores for inf and str enthesitis, BE, and NBF in patients aged ≥ 60 years (Figure 1). Additionally, synovitis and TN scores were significantly higher in b/tsDMARDs-exposed patients. Diabetic patients exhibited higher str enthesitis but lower BE scores compared to non-diabetic patients. Other contextual factors did not show significant differences in US scores.
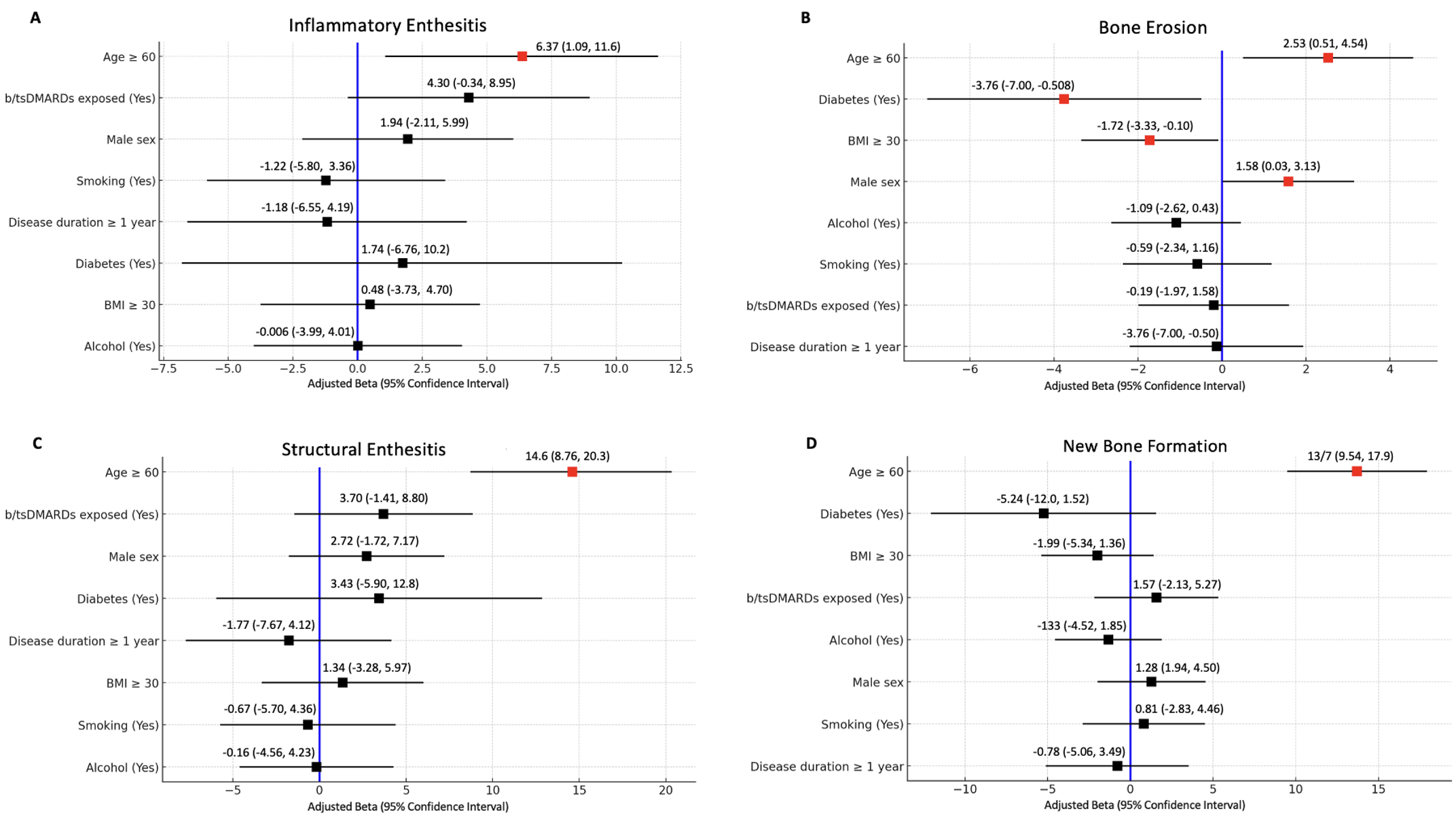
Multivariable analysis (Figure 2) revealed that age ≥ 60 was independently associated with higher scores for inf and str enthesitis (adjusted β 6.37 and 14.6, respectively, p < 0.05). Similarly, b/tsDMARDs-exposure correlated with higher synovitis and TN scores (adjusted β 12.8 and 5.95, respectively, p < 0.05). Other significant associations included age ≥ 60 (adjusted β 2.53), male sex (adjusted β 1.58), BMI ≥ 30 (adjusted β -1.72), and diabetes (adjusted β -3.76) with BE scores. Notably, age ≥60 was also associated with increased NBF scores (adjusted β 13.7, p < 0.001).
Conclusion: Older age consistently correlated with more severe inf and str US lesions, suggesting an association between age and a more severe PsA phenotype or potential overlap with age-related joint abnormalities such as osteoarthritis. The higher synovitis and TN scores observed in b/tsDMARDs-exposed patient may indicate the role of these treatments as severity markers. These findings highlight the importance of integrating patient demographics and treatment history in PsA sonographic assessments to facilitate more personalized management strategies and improve patient outcomes.
To cite this abstract in AMA style:
Lucas Ribeiro A, Thib S, Cui K, Koppikar S, Eder L. Association of Contextual Factors with Sonographic Inflammatory and Structural Phenotypes in Psoriatic Arthritis Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-contextual-factors-with-sonographic-inflammatory-and-structural-phenotypes-in-psoriatic-arthritis-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-contextual-factors-with-sonographic-inflammatory-and-structural-phenotypes-in-psoriatic-arthritis-patients/