Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Community mobility (the extent to which individuals move independently throughout their community) is suboptimal among those with SLE, particularly for those who are Black, have less education, or have higher disease activity. Here, we aimed to explore the association of neighborhood deprivation with community mobility in a population-based U.S. cohort of individuals with validated SLE.
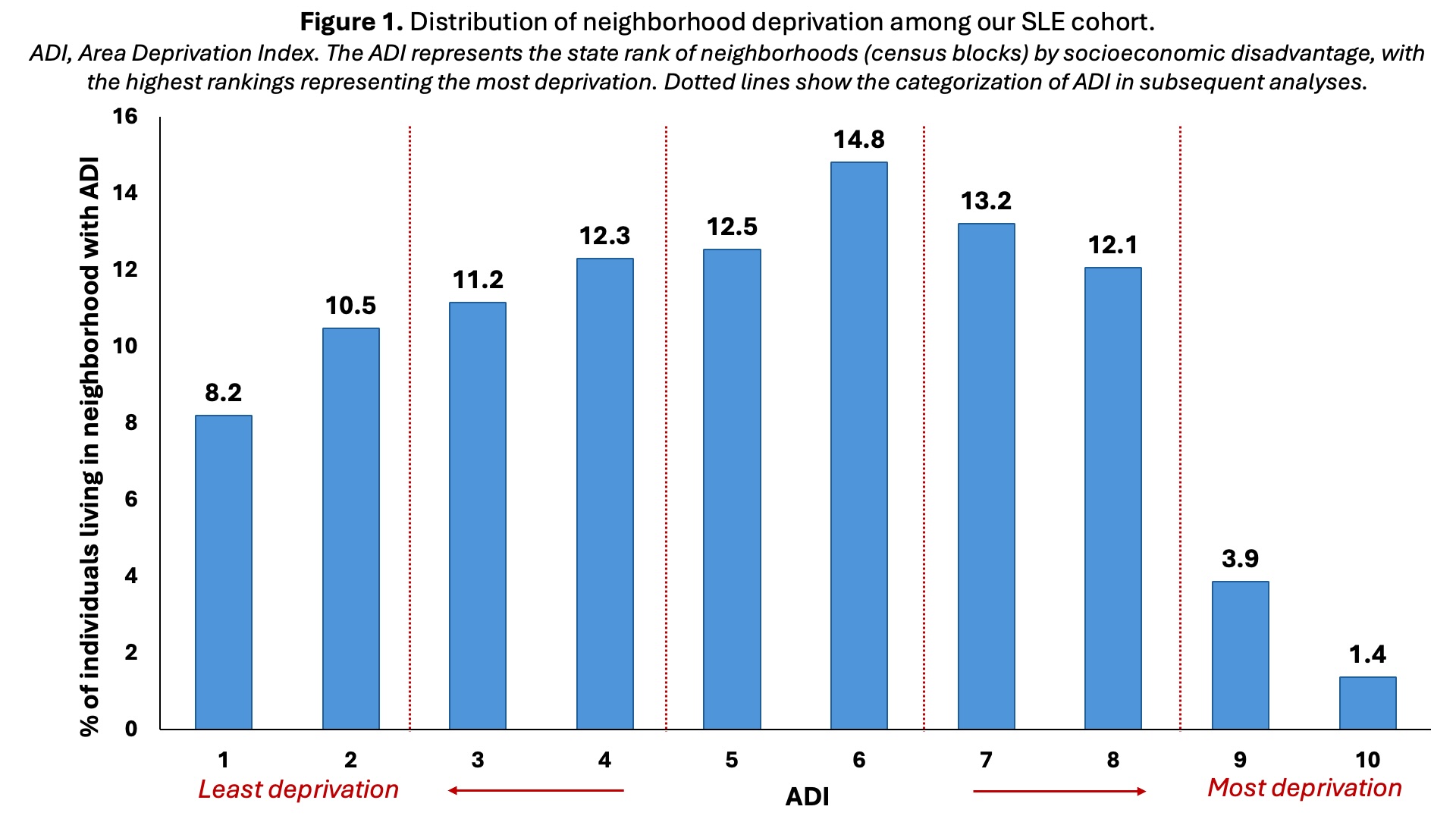
Methods: Participants were recruited (10/2019-5/2022) from the Georgians Organized Against Lupus cohort. Community mobility was measured via the University of Alabama at Birmingham Life Space Assessment (LSA), which asks participants to report how far and how often they have traveled to life-space “levels” (e.g., home, neighborhood) and how much help they needed to reach the levels (score range, 0-120; higher scores=higher and more independent community mobility). We defined unrestricted community mobility as reaching the neighborhood level or beyond, at least weekly and without assistance. Neighborhood deprivation was assessed with the Area Deprivation Index (ADI), a state-based rank of deprivation (including income, education, employment, and housing quality), ranging from 1 (least deprivation) to 10 (most deprivation); these data were linked via census block of participant residential addresses. Descriptive statistics were calculated, and ADI was categorized based on its distribution (Figure 1). We used multivariable linear and logistic regression with adjustment for demographic and clinical variables to estimate the associations between categorized ADI and LSA score and between ADI and unrestricted community mobility, respectively.
Results: Among 447 participants (mean age, 46; 92% female and 82% Black), the median ADI was 5 (25th-75th percentiles, 3-7); 8.2% and 1.4% lived in neighborhoods with the least and most deprivation, respectively (Figure 1). Both the LSA score and the percentage with unrestricted community mobility were highest among individuals living in the least deprived neighborhoods and lowest for those in the most deprived neighborhoods (Figure 2). In unadjusted analyses (Table 1), LSA scores for those living in neighborhoods with ADI 3-4, 5-6, 7-8, and 9-10 were 18, 20, 16, and 29 points lower, respectively, than scores for those living in the least deprived neighborhoods. Similarly, those living in neighborhoods with ADI 3-4, 5-6, 7-8, and 9-10 had 61%, 52%, 56%, and 85% lower odds of having unrestricted community mobility. These associations were similar in direction but attenuated with adjustment for individual demographics and clinical factors.
Conclusion: In our population-based cohort, we found individuals with SLE who were living in neighborhoods with any deprivation—and especially those living in neighborhoods with the most deprivation—had substantially less community mobility than those living in the least deprived neighborhoods. Although some of these differences may be explained by individual characteristics, our results suggest that elicitation of neighborhood factors could be helpful in addressing restrictions in community mobility, which in turn may improve physical and mental health, quality of life, and social participation among those with SLE.
To cite this abstract in AMA style:
Plantinga L, Bowling C, Lim S, Katz P, Yazdany J. Association of Area Socioeconomic Deprivation with Community Mobility in a Diverse Cohort of Individuals with SLE [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-of-area-socioeconomic-deprivation-with-community-mobility-in-a-diverse-cohort-of-individuals-with-sle/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-area-socioeconomic-deprivation-with-community-mobility-in-a-diverse-cohort-of-individuals-with-sle/

.jpg)
.jpg)