Session Information
Date: Monday, November 11, 2019
Title: 4M117: RA – Treatments III: Cardiovascular Disease & Readmissions (1890–1895)
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: The impact of immunosuppression on post-operative outcomes in rheumatoid arthritis (RA) has primarily been studied in patients undergoing joint replacement surgery. We aimed to evaluate the impact of glucocorticoids and biologics on outcomes after other major surgeries.
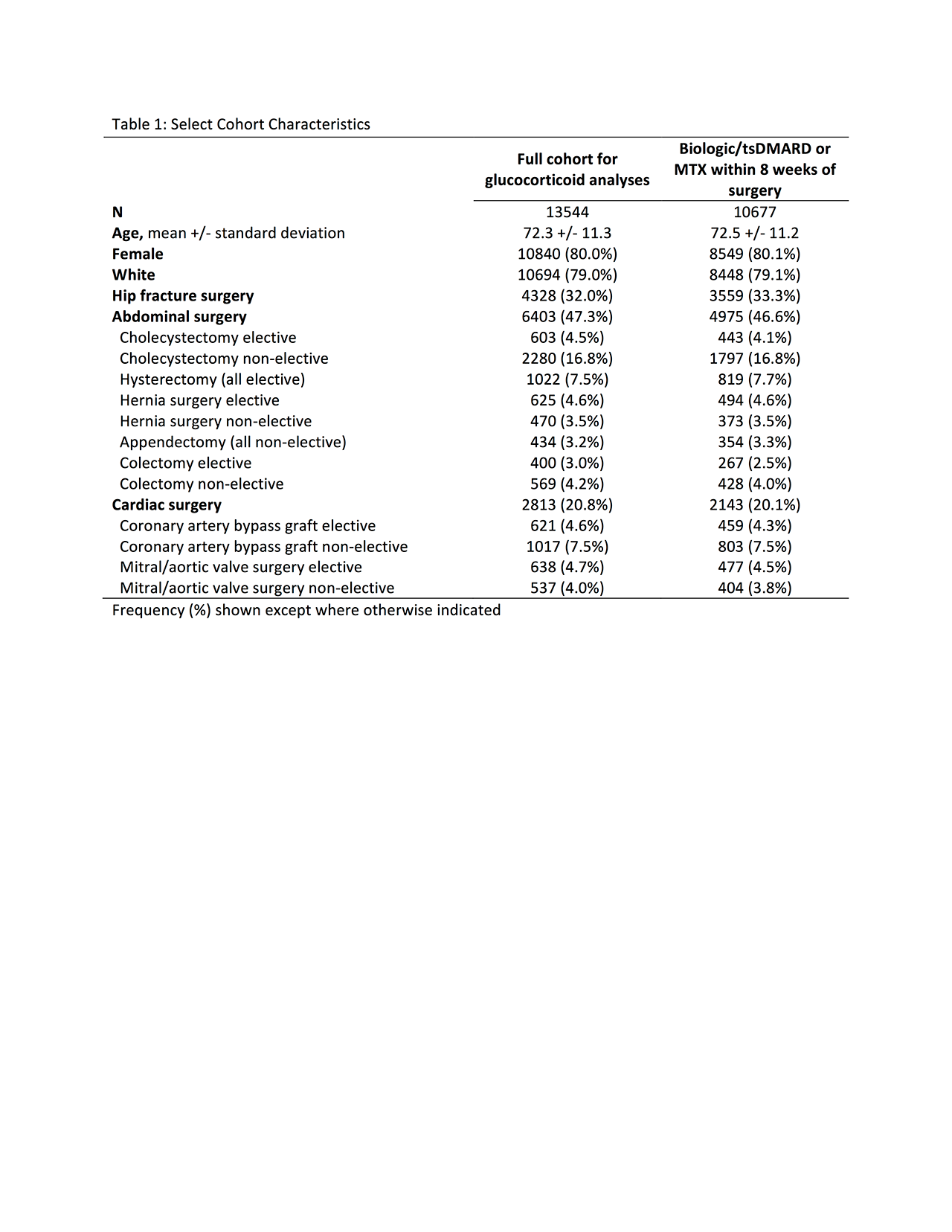
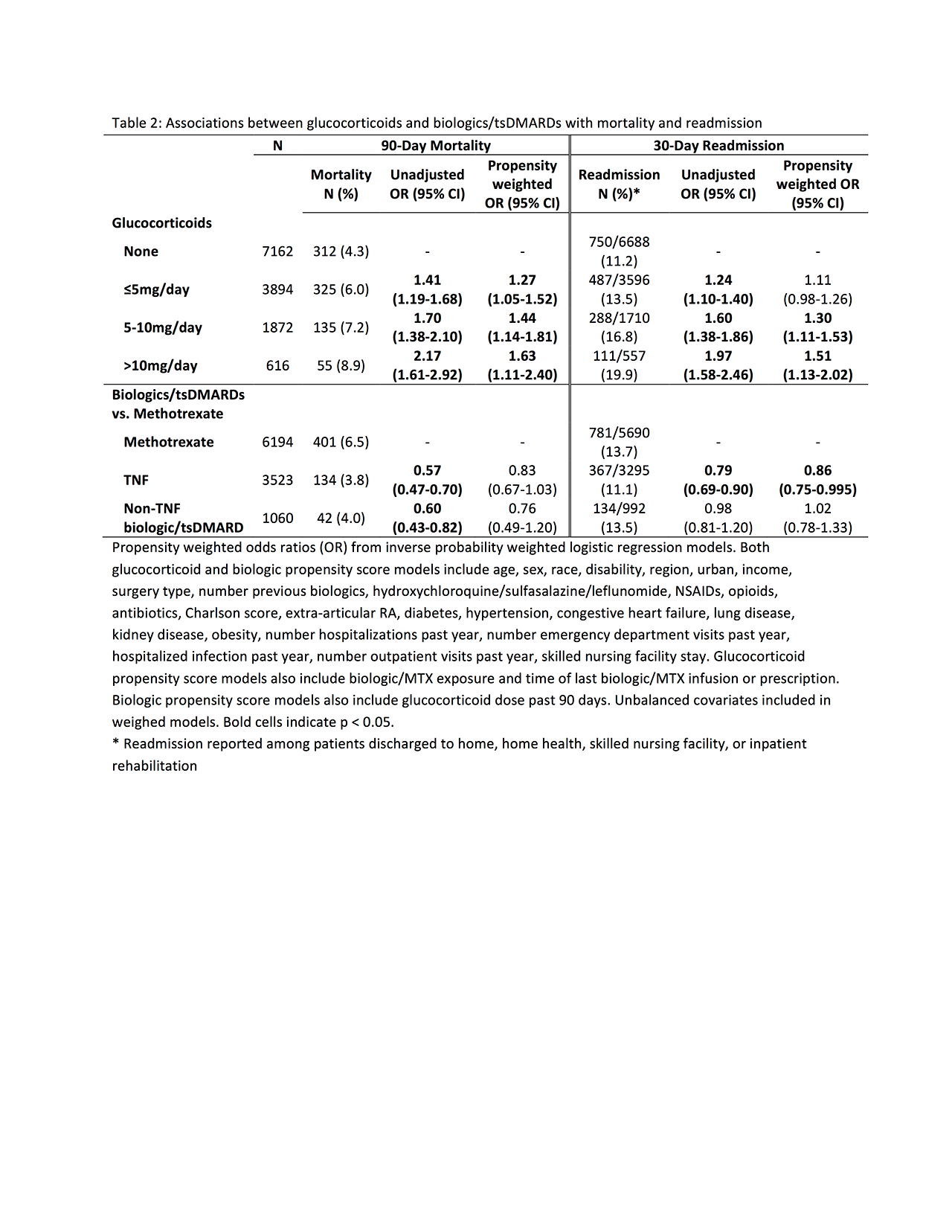
Methods: Using Medicare claims data 2006-2015 we identified adults with ≥2 diagnoses of RA who received methotrexate, a TNF inhibitor, abatacept, rituximab, tocilizumab, or tofacitinib within 6 months before major surgery and had 1 year of continuous prior Medicare enrollment (baseline). Hip fracture repair, abdominal surgeries (cholecystectomy, hysterectomy, hernia surgery, appendectomy, colectomy for diverticular disease), and cardiac surgeries (coronary artery bypass graft, mitral or aortic valve surgery) were identified based on primary ICD-9 procedure codes from inpatient hospitalization using established definitions. Patients with malignancy or HIV and patients with another major surgery within 6 months were excluded. Inverse probability weighted logistic regression models assessed association between average glucocorticoid dose in the 90 days before surgery (none, ≤5mg, 5-10mg, >10mg) and risk of 90-day mortality and 30-day readmission (among patients discharged to home, skilled nursing facility, or inpatient rehabilitation). Propensity score models included surgery type, elective vs. non-elective surgery, demographics, and measures of healthcare utilization, comorbidities, and previous infection during the baseline period. Separate models with recalculated propensity scores compared risk of these outcomes in patients receiving a biologic or targeted synthetic DMARD (tsDMARD) vs. patients exposed to methotrexate without biologics/tsDMARDs, requiring patients to have an infusion or prescription within 8 weeks before surgery.
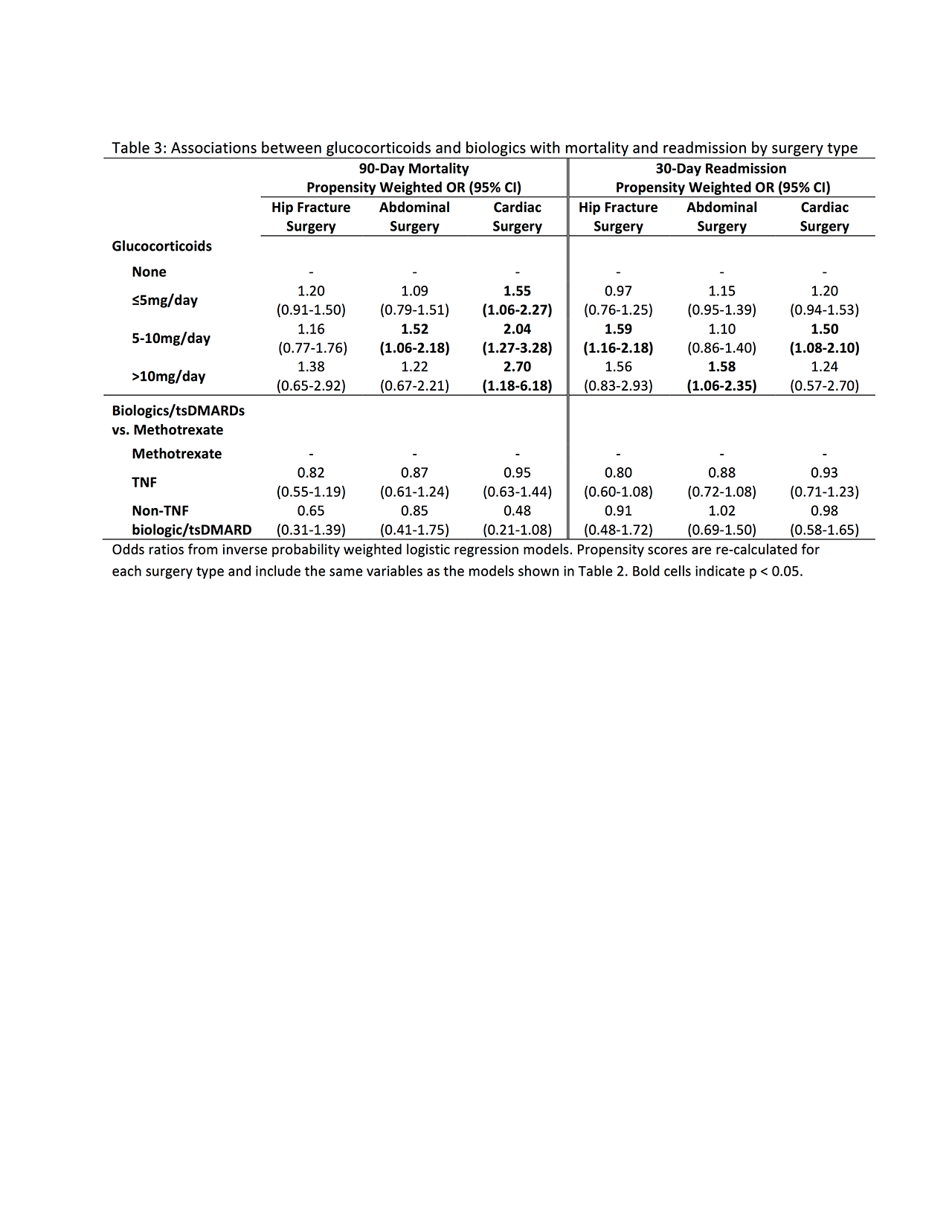
Results: We identified 13544 surgeries meeting all inclusion and exclusion criteria, including 4328 hip fracture surgeries, 6403 abdominal surgeries, and 2813 cardiac surgeries. Glucocorticoids were associated with a dose-dependent increase in the risk of 90-day mortality and 30-day readmission, although associations were partially attenuated in propensity weighted models (Table 2). Associations with mortality were strongest among patients undergoing cardiac surgery, while associations with 30-day readmission were similar across surgeries (Table 3). Among the 10677 (78.8%) of patients who received their biologic/tsDMARD or methotrexate within 8 weeks of surgery, we found no significant increase in the risk of 90-day mortality or 30-day readmission in patients receiving a TNF or patients receiving a non-TNF biologic/tsDMARD vs. patients receiving methotrexate, with similar results across surgery types (Tables 2-3).
Conclusion: Glucocorticoids are associated with greater risk of adverse outcomes after major surgery, especially at higher doses. Recent exposure to biologics/tsDMARDs, however, is not associated with increased mortality or readmission.
To cite this abstract in AMA style:
George M, Baker J, Winthrop K, Chen L, Wu Q, Xie F, Curtis J. Association Between Rheumatoid Arthritis Treatment and the Risk of Death or Readmission After Major Surgery [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/association-between-rheumatoid-arthritis-treatment-and-the-risk-of-death-or-readmission-after-major-surgery/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-rheumatoid-arthritis-treatment-and-the-risk-of-death-or-readmission-after-major-surgery/